Is it wise to vaccinate?John Jacobs, 14 november 2020. |
SARS-2 has a special relation with the immune system. Some people are infected, produce virus, contaminate others, but do not become ill themselves. Others have an immunological response and become flu-like. A minority mounts a strong albeit less efficient immune response failing to neutralize the virus and develops a life-threatening disease. COVID-19 is a virus mediated immune pathology. Immune pathology implies that the immune reaction is causing the disease, in this case triggered by a virus infection. The combination of an immune response ineffective for virus clearance, yet strong enough to cause serious damage yield paradoxes with impact on population health.
Immune paradox
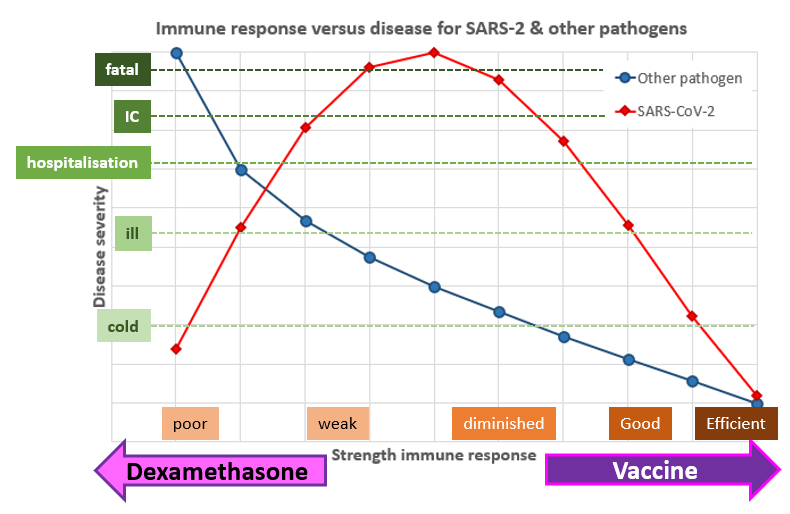
The immune system confers protection against most pathogens. In general, a stronger the immune response yields less disease symptoms. This relation is much more complex for SARS-CoV-2 (Figure 1). People with efficient immune responses do not become ill, but those with poor immune response also not. People with diminished immune responses are most severely affected by the disease, who has an even weaker immune response will become less ill. This paradox can be attributed to the virus immune pathology. This is underlined by the findings that reinfection can be even more severe (see Transient immunity) and that immune suppression with dexamethasone is the best therapy for IC patients with COVID-19.
The immune paradox for coronaviruses changes our understanding of disease, treatment, vaccine development, and is also crucial for strategic consideration on testing and controlling the epidemic.
The immune paradox for coronaviruses changes our understanding of disease, treatment, vaccine development, and is also crucial for strategic consideration on testing and controlling the epidemic.
Figure 1. Immune response versus disease for SARS-2 (red diamonds) and other viruses (blue circle).
Oversimplified version in 1 dimension only. COVID and immunity has a more balanced view on immunity. Dexamethasone decreases immune responsiveness and has a positive effect on IC patients. Vaccination boosts immunity and could prevent disease in patients. However, in people with a poor or bad immune response, boosting of immunity could cause exacerbation of COVID-19.
Oversimplified version in 1 dimension only. COVID and immunity has a more balanced view on immunity. Dexamethasone decreases immune responsiveness and has a positive effect on IC patients. Vaccination boosts immunity and could prevent disease in patients. However, in people with a poor or bad immune response, boosting of immunity could cause exacerbation of COVID-19.
Transient immunity
Immunity against most viruses, like influenza, is often for life. The next time someone is infected with the influenza, it is a different immunological type (serotype), with relevant mutations compared to the previous one. If not, the virus is neutralized by the immune response in immune people.
Coronaviruses tell a different tale. Their story is known because the cause the common cold every year again with the same strains of four corona cold viruses. In case of SARS-1 and MERS only a few people were infected so nobody was reinfected. Anti-SARS1 antibodies wane within a rather short time. It should be noted that antibodies are not considered a reliable indicator for immunity to SARS-2 and this relation has not been investigated for SARS-1.
It is not easy to prove reinfection since both virus strains should differ sufficiently from each other. Thus, someone should be infected in two different ways by two different virus strains. Studies show many confirmed SARS-2 reinfections, including young health people (Tillet, To, Gupta, Mulder, Larson, Bonifacio, van Elslande, AlFehaidi, Lafaie) and many reviews exists (Ledfort, Dao, Kim, Newsweek, BNO news). Reinfections are no exceptions and it is alarming that a second infection generally does not result in milder, but most often a more severe disease.
Also, HIV has reinfections (technically superinfection, since the first was unresolved). Reinfection implies that immunity after the first infection either was insufficient or wane too early. This is also challenge for vaccine development. Antibodies failed to prevent HIV reinfection but seemed to facilitate it.
Considering SARS-2 ability to reinfect people the virus is like to stay among us, similar to the corona cold viruses. This stresses the crucial role for test, trace and isolate (TTI) to prevent contamination and/or vaccination to prevent infection. Disease can be treated in an early or late stage with therapies like interferon and dexamethasone, respectively.
Coronaviruses tell a different tale. Their story is known because the cause the common cold every year again with the same strains of four corona cold viruses. In case of SARS-1 and MERS only a few people were infected so nobody was reinfected. Anti-SARS1 antibodies wane within a rather short time. It should be noted that antibodies are not considered a reliable indicator for immunity to SARS-2 and this relation has not been investigated for SARS-1.
It is not easy to prove reinfection since both virus strains should differ sufficiently from each other. Thus, someone should be infected in two different ways by two different virus strains. Studies show many confirmed SARS-2 reinfections, including young health people (Tillet, To, Gupta, Mulder, Larson, Bonifacio, van Elslande, AlFehaidi, Lafaie) and many reviews exists (Ledfort, Dao, Kim, Newsweek, BNO news). Reinfections are no exceptions and it is alarming that a second infection generally does not result in milder, but most often a more severe disease.
Also, HIV has reinfections (technically superinfection, since the first was unresolved). Reinfection implies that immunity after the first infection either was insufficient or wane too early. This is also challenge for vaccine development. Antibodies failed to prevent HIV reinfection but seemed to facilitate it.
Considering SARS-2 ability to reinfect people the virus is like to stay among us, similar to the corona cold viruses. This stresses the crucial role for test, trace and isolate (TTI) to prevent contamination and/or vaccination to prevent infection. Disease can be treated in an early or late stage with therapies like interferon and dexamethasone, respectively.
Vaccination paradox
The immune system has evolved to neutralize viruses by innate immunity, antibodies and cellular immunity. Viruses evolved various escape mechanisms to avoid immune neutralization prior reinfecting the next host. Vaccination and hygiene have helped mankind to beat many infectious diseases. Some vaccines prevent infection, and most decrease disease severity. Often these are combined and generally it can be viewed as: the stronger the immune response, the lesser the disease.
But not every developed vaccine is effective, especially diseases caused by coronaviruses, flaviviruses and HIV are difficult to prevent, even with vaccines inducing strong immune responses. A corona vaccine exacerbated the disease by the strong immune response. A moderate immune response against SARS-2 causes a disease but does not clear the infection. Vaccination boosts anti-virus immune responses. This may be desired in people with weak immune response but might also exacerbate the disease.
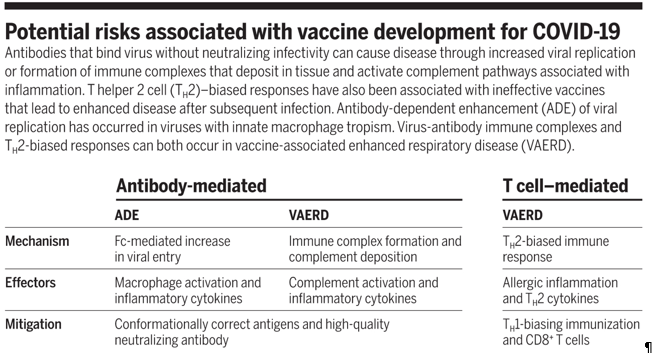
At an early stage of the epidemic, immunologists pointed at the contrasting effects of vaccination, i.e. antibody-dependent enhancement of viral replication (ADE) and vaccine-associated enhancement of respiratory disease by immune complexes and complement formation (VAERD) (Figure 2). Neither is a direct consequence of vaccination but could occur if a vaccinated person becomes infected with the virus. This would imply that the vaccine would do what has been tried to prevent: vaccinated people have more severe disease after infection. This is foreshadowed by enhancement of disease in recurrent SARS-2 infections.
ADE might be caused by neutralizing antibodies against the corona Spike protein. This protein is used in all corona vaccines. Neutralizing antibodies mediate ADE with the corona viruses SARS-1 and MERS. ADE is also important for flaviviruses Dengue-, Zika- and West-Nile virus, and also for HIV (AIS virus). ADE hampers the development of safe and effective vaccines, and for most of these viruses, no working vaccines have yet been registered (SARS-1, MERS, HIV, West-Nile, Zika-virus). Dengue virus is the only exception so far.
But not every developed vaccine is effective, especially diseases caused by coronaviruses, flaviviruses and HIV are difficult to prevent, even with vaccines inducing strong immune responses. A corona vaccine exacerbated the disease by the strong immune response. A moderate immune response against SARS-2 causes a disease but does not clear the infection. Vaccination boosts anti-virus immune responses. This may be desired in people with weak immune response but might also exacerbate the disease.
At an early stage of the epidemic, immunologists pointed at the contrasting effects of vaccination, i.e. antibody-dependent enhancement of viral replication (ADE) and vaccine-associated enhancement of respiratory disease by immune complexes and complement formation (VAERD) (Figure 2). Neither is a direct consequence of vaccination but could occur if a vaccinated person becomes infected with the virus. This would imply that the vaccine would do what has been tried to prevent: vaccinated people have more severe disease after infection. This is foreshadowed by enhancement of disease in recurrent SARS-2 infections.
ADE might be caused by neutralizing antibodies against the corona Spike protein. This protein is used in all corona vaccines. Neutralizing antibodies mediate ADE with the corona viruses SARS-1 and MERS. ADE is also important for flaviviruses Dengue-, Zika- and West-Nile virus, and also for HIV (AIS virus). ADE hampers the development of safe and effective vaccines, and for most of these viruses, no working vaccines have yet been registered (SARS-1, MERS, HIV, West-Nile, Zika-virus). Dengue virus is the only exception so far.
Figure 2. Putative risks from COVID-19 vaccination.
Immune overstimulation
Experimental animal research for reinfection is difficult because macaques are protected against reinfection with SARS-CoV-2. These and other animals have a difference in immunology than humans, as has been shown by the cytokine storm caused by TGN1412. These monkeys do not suffer from this, while this sepsis is fatal in humans. This or another immunological mechanism could cause the different immunity to SARS-CoV-2 in humans and macaques. Evidently, animal experiments failing to mimic human disease correctly, will not yield an adequate prediction for humans. In the Dutch Federation of Medical Scientific Society, we organized in 2016 a Federa-day on Health(y) science, increasing value, reducing waste. Or as the speakers stressed: sloppy methodology yields little value for patients.
Non-sterile immunity
From a clinical point of view viruses cause two sorts of infections: symptomatic and asymptomatic. In epidemiology infections without symptoms are the most dangerous since healthy people will be unrestricted in contacts with other people and contaminate these. Most infections induce immunity against the disease and often also sterilizing immunity against the infection. Immunity against corona viruses is short lived and generally not sterilizing. SARS-2 infections are frequently found without symptoms and even reinfection can be asymptomatic. People who do not become ill from SARS-2 can excrete the virus for a prolonged period and thus infect others. This non-sterile immunity could have an important role in spreading the disease. People without symptoms have no incentives for quarantine unless TTI identifies them as such.
How long will protection last?
This is the one-million-dollar question, but the answer might be different for each type of vaccination and immunity. The large number of reinfections suggest that the average immunity is short lived after infection, i.e. less than one year. The vaccine trials focused on early protection, i.e. the first few months after vaccination, since in this time frame about 1% of participants acquire disease. When a predetermined number of disease cases has been counted, the trial code is decoded, and the results are analysed. The difference found reflects the first few months after vaccination and the difference between the vaccine-treated and control groups. The trial results are thus ignorant considering protection after 6 or 12 months after vaccination. Immunological knowledge on SARS-2 immunity is lacking –which antibodies and/or cellular mediators play a role? – thus it is hard to measure immunity. If immunity after natural infection is an indication for the longevity of immunity, people might need multiple vaccination each year. In the Netherlands it is estimated that it would take about a year to vaccinate everyone, the UK is more optimistic and estimates six months. It is clear we cannot protect everyone with vaccination yet.
Protected against what?
Pfizer and BioNTech cheered in their press release that their COVID-19 vaccine is 90% effective. A good average against disease in medicine does not exclude putative negative effects for some people. The world did not hurry to vaccine development to fight flu-like complaints in people, but because of mortality and high morbidity after COVID-19. None of the seven vaccine trials, studies protection from severe disease as primary outcome.
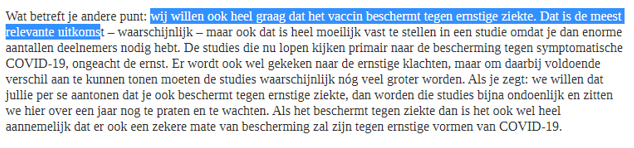
I was disappointed by the vision of the Dutch Medicines Evaluation Board (CBG) (Figure 3). Objectively, this judgement does not increase the value of a COVID-19 vaccine beyond that of a vaccine against the cold. A vaccine unable to prevent serious disease of mortality does not have a high priority. I do underscore that a COVID-19 vaccine could do much more in theory, like preventing serious disease and mortality. However, the current vaccine trials did not show this. This undermines the ground to vaccinate whole Europe without any further clinical trials.
I was disappointed by the vision of the Dutch Medicines Evaluation Board (CBG) (Figure 3). Objectively, this judgement does not increase the value of a COVID-19 vaccine beyond that of a vaccine against the cold. A vaccine unable to prevent serious disease of mortality does not have a high priority. I do underscore that a COVID-19 vaccine could do much more in theory, like preventing serious disease and mortality. However, the current vaccine trials did not show this. This undermines the ground to vaccinate whole Europe without any further clinical trials.
Figure 3. CBG on desired efficacy of vaccination.
Their reply tells that they want protection against serious disease, since this is the most relevant outcome, but do not know how this could be studied without designing huge trials. The conclude by assuming that protection against disease would imply protection against serious disease and mortality.
Their reply tells that they want protection against serious disease, since this is the most relevant outcome, but do not know how this could be studied without designing huge trials. The conclude by assuming that protection against disease would imply protection against serious disease and mortality.
Who do we want to protect?
The advices of the Dutch health council and the EU contain prioritization strategies to protect certain groups of people. These choices appear logic at first sight but are built on the quicksand of unproven and unspoken assumptions. Scientific advice without common sense requires a thorough discussion.
The second priority group contains the care workers. Personal protection from some disease is appreciated but should not have a major urgency. To prevent serious disease of mortality should be an urgency, but we have no evidence that these vaccines could do this. Another unspoken assumption is the idea vaccination of health care workers might prevent that infected healthcare workers contaminate vulnerable people. Indeed, for most virus’ immunity implies sterile immunity, but I have shown indication that SARS-2 immunity might be an exception to this rule. If this also holds for SARS-2 immunity after vaccination, it might protect vaccinated caregivers from disease, while the contaminate their vulnerable patients.
The first group are the vulnerable people, i.e. over 60 years old and people with various morbidities. The motivation to vaccinate these is clear: these people have an increase risk on COVID-19 mortality and serious morbidity. However, none of the current vaccination trials studies the prevention of hospitalization, IC-uptake or mortality as primary outcome. Immunity is diminished in elderly and vaccination might be less effective for them. However, it has not been studied if the elderly are protected after vaccination.
The second priority group contains the care workers. Personal protection from some disease is appreciated but should not have a major urgency. To prevent serious disease of mortality should be an urgency, but we have no evidence that these vaccines could do this. Another unspoken assumption is the idea vaccination of health care workers might prevent that infected healthcare workers contaminate vulnerable people. Indeed, for most virus’ immunity implies sterile immunity, but I have shown indication that SARS-2 immunity might be an exception to this rule. If this also holds for SARS-2 immunity after vaccination, it might protect vaccinated caregivers from disease, while the contaminate their vulnerable patients.
The first group are the vulnerable people, i.e. over 60 years old and people with various morbidities. The motivation to vaccinate these is clear: these people have an increase risk on COVID-19 mortality and serious morbidity. However, none of the current vaccination trials studies the prevention of hospitalization, IC-uptake or mortality as primary outcome. Immunity is diminished in elderly and vaccination might be less effective for them. However, it has not been studied if the elderly are protected after vaccination.
Too valuable to waste
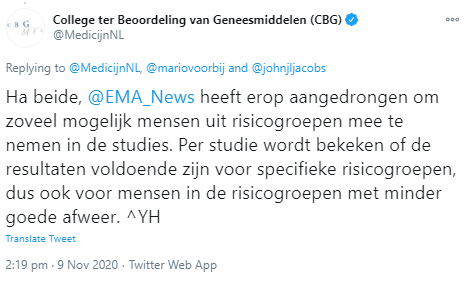
The British, Dutch and probably some other European governments want a rapid introduction of COVID-19 vaccination with all putative risks. A rapid introduction from a production that still needs to be upscaled could take a year. I conclude that vaccination could be useful against COVID-19, but still has too many uncertainties considering vaccine safety. If a vaccine induces the wrong immune response, it might be detrimental. The European Medicines Agency (EMA) urged to include as many as possible people from risk groups in the studies (Figure 4). A percentage of these will likely have a serious disease after COVID-19 infection. The current vaccine trials are statistically underpowered for this analysis, so they might not answer the question if vaccination ameliorates or exacerbates disease upon infection. From a methodological perspective, this approach is suboptimal and insufficient to protect peoples lives.
What would be a better approach? The Federa-day in 2017 focussed at experiments on humans and animals: too valuable to waste. It is crucial that relevant participants are included in the trials. Cardiovascular disease is an important risk factor for COVID-19 mortality. Age is an important predictor in its risk modulation. Age might also be crucial in the COVID-19 vaccine trials, and thus should be properly introduced. Without careful research on human, everyone will be and remain subject of treatments without evidence. Immunologic research for probiotics showed that an effect could be positive for mild disease, but negative at a severe infection.
Should we wait another year, as the CBG fears (Figure 3)? No, not at all. It makes perfectly sense to use the ordered vaccines in a double-blind randomized clinical phase 3 trial for vulnerable patients. The primary outcome should be severe morbidity, i.e. hospitalization and IC uptake and mortality in this group. Considering Europe’s anti-COVID-19 strategies there will be plenty of infections in the third COVID-19 wave which is to be expected, to set up a study, inject everyone, and yield sufficient sever COVID-19 to evaluate if vaccination has a positive or negative effect. Immediately when the efficacy in preventing serious disease in vulnerable people is known, all vulnerable people could be given or withheld the vaccination. Should it be ineffective or detrimental, at least we did not vaccinate too many people. Should it be protective, we could rapidly vaccinate everyone, including those that were not vaccinated in the studies. This will allow to protect people the maximally according to the best evidence-based medicine and avoids that wrong assumption drastically waste human lives. Or as I could summarize both Federa-days: human lives are too valuable to waste with sloppy science.
What would be a better approach? The Federa-day in 2017 focussed at experiments on humans and animals: too valuable to waste. It is crucial that relevant participants are included in the trials. Cardiovascular disease is an important risk factor for COVID-19 mortality. Age is an important predictor in its risk modulation. Age might also be crucial in the COVID-19 vaccine trials, and thus should be properly introduced. Without careful research on human, everyone will be and remain subject of treatments without evidence. Immunologic research for probiotics showed that an effect could be positive for mild disease, but negative at a severe infection.
Should we wait another year, as the CBG fears (Figure 3)? No, not at all. It makes perfectly sense to use the ordered vaccines in a double-blind randomized clinical phase 3 trial for vulnerable patients. The primary outcome should be severe morbidity, i.e. hospitalization and IC uptake and mortality in this group. Considering Europe’s anti-COVID-19 strategies there will be plenty of infections in the third COVID-19 wave which is to be expected, to set up a study, inject everyone, and yield sufficient sever COVID-19 to evaluate if vaccination has a positive or negative effect. Immediately when the efficacy in preventing serious disease in vulnerable people is known, all vulnerable people could be given or withheld the vaccination. Should it be ineffective or detrimental, at least we did not vaccinate too many people. Should it be protective, we could rapidly vaccinate everyone, including those that were not vaccinated in the studies. This will allow to protect people the maximally according to the best evidence-based medicine and avoids that wrong assumption drastically waste human lives. Or as I could summarize both Federa-days: human lives are too valuable to waste with sloppy science.
Figure 4. CBG states that the EMA advised to include as many vulnerable people as possible in the vaccine trials.
John Jacobs
14.11.2020
14.11.2020