COVID-19
Special immunity
John Jacobs, 6th March 2021.
Immune factors
Airway viruses have a paradoxical relationship with the immune system. Early in infections, people have high virus titers but less disease due to minimal immune responses. Increasing the immune response will be the onset of the disease. Respiratory tract infections have a special immunology and SARS-2 goes the extremes: fatal disease is caused by an inefficient but strong immune response. Thus it is crucial to distinguish between different immune components and their roles:
- Innate immunity. The natural resistance of healthy tissue that tackles harmful viruses and bacteria at an early stage. When amplified it could make you sick.
- Early antibodies (IgM). Antibodies in the circulation that are temporarily present with limited efficacy, due to limited binding strength.
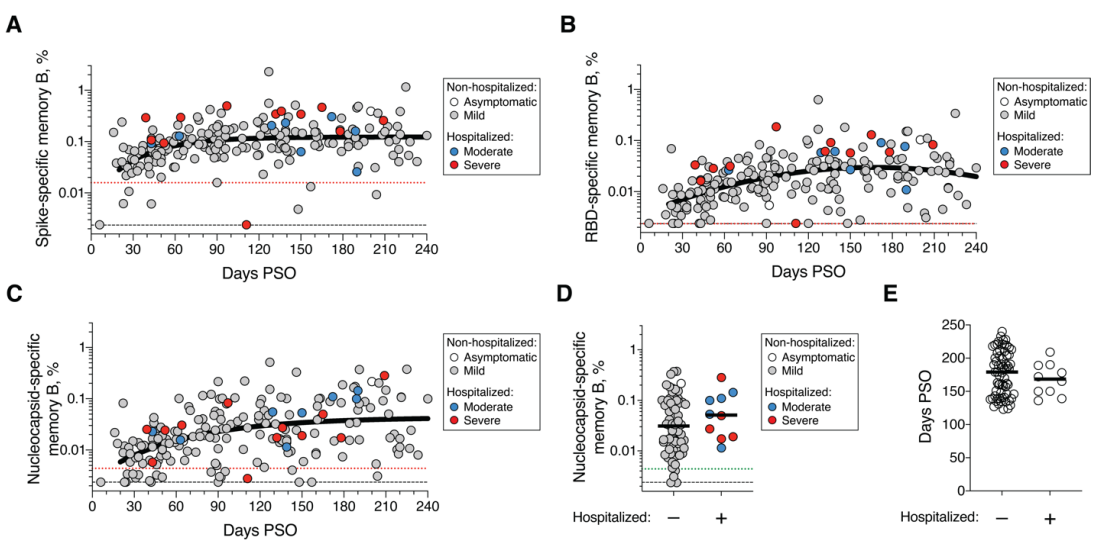
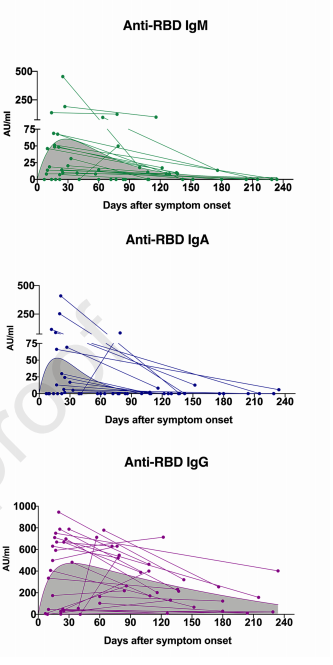
- Common antibodies (IgG). Antibodies in the circulation that can neutralize the virus directly and / or label it for phagocytes to eat the virus. The latter may occasionally cause infection of those immune cells. People with more antibodies have more symptoms (Figure 1). So antibodies may not only protect, but also have a role in the disease.
- Mucosal antibodies (IgA). Antibodies that are transported from the normal circulation to the mucous membranes of the respiratory tract and the gastrointestinal tract. These antibodies are necessary to prevent someone from becoming infected and contagious - called sterilizing immunity.
- Cytotoxic T cells. CD8 T cells that can eliminate virus-infected cells and prevent virus production by these cells.
- Helper T cells. CD4 T cells that assist CD8 T cells and / or B cells. These are required for B cells to switch to IgG and/or IgA production.
Figure 1. Antibody memory after COVID-19
Immunity against SARS-2
Type 1 interferon (α, β) are an efficient early defense that prevents infection.
When infection is not prevented, most people with mild SARS-2 infection have both neutralizing antibodies and T cell responses.
When do people become seriously ill? Good T cell responses seem to prevent serious disease. People with poor T cell responses, i.e., often elderly, sometimes acquire serious disease. Most often when they have strong antibody responses. It is suggested that neutralizing antibodies could play a role, but antibodies could also prevent the cellular virus infection.
High numbers of CD4 and / or CD8 T cells protect against disease. This illustrates that, as with most viral infections, including influenza, cellular immunity provides the most important protection against disease. However, cellular immunity does not eliminate free virus and will only infiltrate tissues after the infection has started, so it will never provide sterilizing immunity.
High IgG antibody titers seem to be no problem prior infection since these antibodies may prevent the symptomatic infection. But when IgG antibodies are produced during disease, it is associated with worse outcome. It cannot be ruled out that antibodies may aggravate the disease by enhancing the inflammatory response and spreading the virus through antibody-mediated infection of myeloid blood cells.
Antigen-specific immunity to infection prevents disease, but not infection. The T cells and IgG or IgM antibodies do not enter the epithelial tissues beyond the basement membrane. Only IgA antibodies can induce sterilizing immunity. IgG antibodies remain for more than six months.
When infection is not prevented, most people with mild SARS-2 infection have both neutralizing antibodies and T cell responses.
When do people become seriously ill? Good T cell responses seem to prevent serious disease. People with poor T cell responses, i.e., often elderly, sometimes acquire serious disease. Most often when they have strong antibody responses. It is suggested that neutralizing antibodies could play a role, but antibodies could also prevent the cellular virus infection.
High numbers of CD4 and / or CD8 T cells protect against disease. This illustrates that, as with most viral infections, including influenza, cellular immunity provides the most important protection against disease. However, cellular immunity does not eliminate free virus and will only infiltrate tissues after the infection has started, so it will never provide sterilizing immunity.
High IgG antibody titers seem to be no problem prior infection since these antibodies may prevent the symptomatic infection. But when IgG antibodies are produced during disease, it is associated with worse outcome. It cannot be ruled out that antibodies may aggravate the disease by enhancing the inflammatory response and spreading the virus through antibody-mediated infection of myeloid blood cells.
Antigen-specific immunity to infection prevents disease, but not infection. The T cells and IgG or IgM antibodies do not enter the epithelial tissues beyond the basement membrane. Only IgA antibodies can induce sterilizing immunity. IgG antibodies remain for more than six months.
Innate immunity
Coronaviruses are known for their seasonal infections and disease in temperate areas: the common cold. In tropical regions they cause this disease all year round. Coronaviruses cause more disease in the winter periods in temperate areas because of:
The innate immune system does not provide immunity against disease unless specific immune responses have been initiated. The general defense directs the direction of the specific immunity, such as T cells and / or various antibodies. Regardless of the season, type 1 interferon (α, β) is an important defense of cells against virus infection. The immune system has many feedback loops and in some people the Interferon β response is blocked. This leads to more serious illness. General or natural defenses in the mucous membranes play a crucial role in preventing the disease and minimizing the infection. In the first weeks after a virus infection or vaccination, type 1 interferon is made. Interferon is made by almost all cells in the body after contact with a virus or after vaccination.
Interferon is effective against SARS-2, but the virus inhibits interferon production, creating a critical balance. Young people with limited interferon would be considered healthy but have a serious risk of COVID-19 related mortality after infection.
- Low temperatures stabilizes the virus.
- Cold and dry air make the mucous membranes more vulnerable.
- Lower vitamin D levels in people since this is produced by the skin when in the sunlight. Vitamin D is lower in the elderly and in dark skin people. Vitamin D3 tablets (recommended daily allowance!) are advised to prevent respiratory RNA virus infections - this includes the coronaviruses. Normal vitamin D levels are important to prevent the disease.
- Air pollution is an important co-factor for infection and disease. Pollution irritates the mucous membranes making them more vulnerable to infection and exacerbating the inflammation.
The innate immune system does not provide immunity against disease unless specific immune responses have been initiated. The general defense directs the direction of the specific immunity, such as T cells and / or various antibodies. Regardless of the season, type 1 interferon (α, β) is an important defense of cells against virus infection. The immune system has many feedback loops and in some people the Interferon β response is blocked. This leads to more serious illness. General or natural defenses in the mucous membranes play a crucial role in preventing the disease and minimizing the infection. In the first weeks after a virus infection or vaccination, type 1 interferon is made. Interferon is made by almost all cells in the body after contact with a virus or after vaccination.
Interferon is effective against SARS-2, but the virus inhibits interferon production, creating a critical balance. Young people with limited interferon would be considered healthy but have a serious risk of COVID-19 related mortality after infection.
Antigen-specific immunity
Antigen-specific immune responses consist of T cells and antibodies produced by B cells. Many studies measure antibody levels without measuring T-cell immune responses. The underlying innate immune responses are similar for B and T-cell responses. Someone with antibodies would have been in contact with the virus or vaccine, which would also induce T cell responses. Since many studies do not look at T-cell status, most antibody papers are difficult to interpret on if immunity is caused by – or T-cells. Despite increased immunity, not all people are protected against reinfection. It is easier to be protected from disease than from infection.
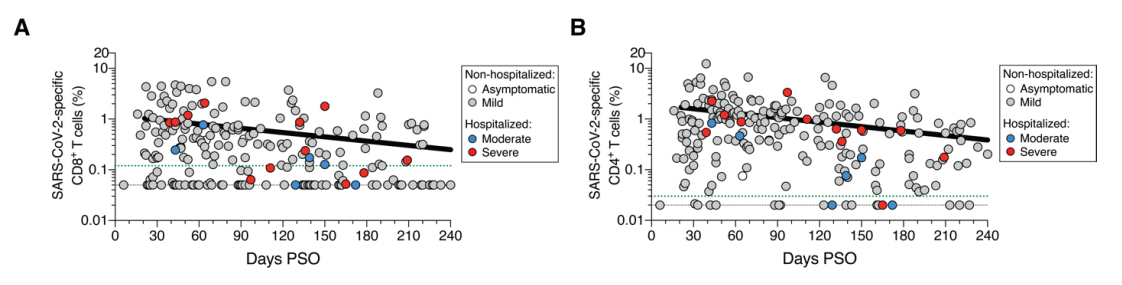
T cells are crucial in the cellular defense. T cell immunity to COVID-19 is strong, especially the CD8 response after mild infection. After infections, the number of T cells decreases. CD4 T cells have a half-life of 3 to 7 months and CD8 T cells from 4 to 9 months. In 1/6 and ¼ of the humans, CD4 and CD8 T cell cytokine responses can no longer be detected after 7 and 9 months, respectively. It is not clear how much T cell responses are needed to have immunity against the disease.
Studies in common cold viruses show that antibody titers increase after infection with a maximum for IgG and IgA about 3 weeks after infection. After about 5 days the symptoms begin and after about 13 days the body produces IgG antibodies. On day 19 after the onset of symptoms, everyone has IgG antibodies. We know from other (corona) viruses that IgA follows a few days later. Antibodies decrease after the disease, especially the decrease in IgM and IgA are strong.
T cells are crucial in the cellular defense. T cell immunity to COVID-19 is strong, especially the CD8 response after mild infection. After infections, the number of T cells decreases. CD4 T cells have a half-life of 3 to 7 months and CD8 T cells from 4 to 9 months. In 1/6 and ¼ of the humans, CD4 and CD8 T cell cytokine responses can no longer be detected after 7 and 9 months, respectively. It is not clear how much T cell responses are needed to have immunity against the disease.
Studies in common cold viruses show that antibody titers increase after infection with a maximum for IgG and IgA about 3 weeks after infection. After about 5 days the symptoms begin and after about 13 days the body produces IgG antibodies. On day 19 after the onset of symptoms, everyone has IgG antibodies. We know from other (corona) viruses that IgA follows a few days later. Antibodies decrease after the disease, especially the decrease in IgM and IgA are strong.
Choose left or right.
Someone started a lecture on analysis with planes that had been shot at in a war but returned. The contemporary hypothesis was that the planes had to be reinforced at the bullet holes. Someone dared to challenge this hypothesis and came up with the alternate hypothesis that aircraft should be protected in places where there were no holes. The argument was that any holes found had not prevented the planes from returning. This story came back as a flashback when I heard the RIVM explanation of antibodies in COVID-19.
RIVM head van Dissel and some other scientists argue that people with mild complaints make less antibodies and thus become less immune. People with few or no symptoms have little or no neutralizing antibodies to SARS-2. Older people have higher antibody titers than young people. People who are admitted to hospital have 10 to 30 times as high antibodies levels than people who can stay out at home. Children are infected just as often and excrete virus just as often but are less often (seriously) ill and have antibodies less often, according to the RIVM.
The WHO rightly states that "no studies have shown that antibodies against SARS-CoV-2 protect against new infection with this virus in humans." An effective innate defense can prevent someone from becoming infected and ill, but if the virus breaks through, the virus-specific immunity must be activated. It consists of two main forms: antibodies and cellular defense. Strong immune responses are seen in severe illness. Apparently, people with a moderate antibody response are still able to avoid becoming seriously ill. This is probably due to cellular defenses.
Scientists debate if high antibody levels in critically ill patients are the cause of, the consequence of, or the protection against serious disease. The first corresponds to the phenomenon of viral immune pathology. The second considers antibodies an epiphenomenon. The third conflicts with the fatal disease associated with high antibody titers. People who are well protected should not die from a disease. These are the main reasons for me to suspect the former.
RIVM head van Dissel and some other scientists argue that people with mild complaints make less antibodies and thus become less immune. People with few or no symptoms have little or no neutralizing antibodies to SARS-2. Older people have higher antibody titers than young people. People who are admitted to hospital have 10 to 30 times as high antibodies levels than people who can stay out at home. Children are infected just as often and excrete virus just as often but are less often (seriously) ill and have antibodies less often, according to the RIVM.
The WHO rightly states that "no studies have shown that antibodies against SARS-CoV-2 protect against new infection with this virus in humans." An effective innate defense can prevent someone from becoming infected and ill, but if the virus breaks through, the virus-specific immunity must be activated. It consists of two main forms: antibodies and cellular defense. Strong immune responses are seen in severe illness. Apparently, people with a moderate antibody response are still able to avoid becoming seriously ill. This is probably due to cellular defenses.
Scientists debate if high antibody levels in critically ill patients are the cause of, the consequence of, or the protection against serious disease. The first corresponds to the phenomenon of viral immune pathology. The second considers antibodies an epiphenomenon. The third conflicts with the fatal disease associated with high antibody titers. People who are well protected should not die from a disease. These are the main reasons for me to suspect the former.
Bitter or sweet antibodies?
Many studies only investigate antibodies because of technical simplicity. However, antibody levels do not inform on T cell responses. If either or both are required for effective virus elimination, studying only one will yield incomplete information. Almost all diseased and infected people have detectable antibodies levels but out of asymptomatic only 1 in 5.
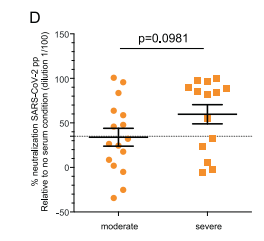
A strong immune response with high antibody levels predicts a serious disease and worse outcome (Figure 2). High titers of neutralizing antibodies correlate positively with high levels of inflammation (CRP) and negatively with the number of white blood cells. Elder patients often have higher levels of neutralizing antibodies than younger patients. These antibodies could be the start of sepsis, the fatal course of COVID-19.
The correlation of antibodies with disease and fatal outcome should be noted since similar neutralizing antibodies against the Spike protein are also induced by vaccines. With other coronaviruses, people with higher antibody levels are probably better protected against infection, and this may also be the case for SARS-2. However, the state prior disease and during disease are not the same.
Some people's immune systems react weakly to the virus and these people can remain infected with high virus titers for a prolonged period without serious illness. As with most respiratory viruses, getting sick is mainly the result of the immune response against the virus, not the virus itself. Becoming ill results in decreasing virus levels.
Fucose is a sugar group that binds to the constant part of most antibodies. Corona patients who end up in the intensive care unit make antibodies without this fucose group, i.e., unfucosylated antibodies. The absence of this sugar group is not seen in people with only mild complaints. These low sugar antibodies provide an extremely powerful and harmful immune response. Normally only ~ 6% of the IgG is unfucosylated, but some people have increased levels of low-sugar antibodies against coronaviruses and other membrane viruses. Non-fucosylated IgG binds more strongly to Fc receptors (FcγRIIIa; CD16). CD16 activation by antibodies enhances cytokine response and is involved in the amplification of the immune response by antigen-antibody complex allergic reactions. Virus endocytosis could also result in infection of leukocytes and spreading the virus. The cytokine storm or sepsis in SARS-2 is the mechanism by which SARS-2 is potentially fatal. The hypothesis that neutralizing antibodies cause virus immune pathology may be refined to low-sugar neutralizing antibodies. While many patients with reduced cellular immunity are more vulnerable to fatal COVID-19, people without antibodies appear to have a milder disease course. Currently the evidence for undesired immune responses point to the unfucosylated IgG.
A strong immune response with high antibody levels predicts a serious disease and worse outcome (Figure 2). High titers of neutralizing antibodies correlate positively with high levels of inflammation (CRP) and negatively with the number of white blood cells. Elder patients often have higher levels of neutralizing antibodies than younger patients. These antibodies could be the start of sepsis, the fatal course of COVID-19.
The correlation of antibodies with disease and fatal outcome should be noted since similar neutralizing antibodies against the Spike protein are also induced by vaccines. With other coronaviruses, people with higher antibody levels are probably better protected against infection, and this may also be the case for SARS-2. However, the state prior disease and during disease are not the same.
Some people's immune systems react weakly to the virus and these people can remain infected with high virus titers for a prolonged period without serious illness. As with most respiratory viruses, getting sick is mainly the result of the immune response against the virus, not the virus itself. Becoming ill results in decreasing virus levels.
Fucose is a sugar group that binds to the constant part of most antibodies. Corona patients who end up in the intensive care unit make antibodies without this fucose group, i.e., unfucosylated antibodies. The absence of this sugar group is not seen in people with only mild complaints. These low sugar antibodies provide an extremely powerful and harmful immune response. Normally only ~ 6% of the IgG is unfucosylated, but some people have increased levels of low-sugar antibodies against coronaviruses and other membrane viruses. Non-fucosylated IgG binds more strongly to Fc receptors (FcγRIIIa; CD16). CD16 activation by antibodies enhances cytokine response and is involved in the amplification of the immune response by antigen-antibody complex allergic reactions. Virus endocytosis could also result in infection of leukocytes and spreading the virus. The cytokine storm or sepsis in SARS-2 is the mechanism by which SARS-2 is potentially fatal. The hypothesis that neutralizing antibodies cause virus immune pathology may be refined to low-sugar neutralizing antibodies. While many patients with reduced cellular immunity are more vulnerable to fatal COVID-19, people without antibodies appear to have a milder disease course. Currently the evidence for undesired immune responses point to the unfucosylated IgG.
Figure 2 Neutralization of SARS-2 by antibodies in people with severe and moderate COVID-19
Antibody maturation and mutations
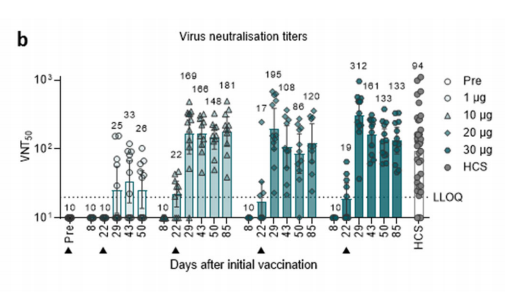
Antibodies become stronger through maturation (see explanation). Mature antibodies bind more strongly to the virus, requiring less antibodies to neutralize the virus. Four weeks after infection or vaccination, people have protective antibodies. Antibody maturation requires antibodies requires antigen or virus. This could be done through a second vaccination, but also happens naturally after an infection (Figure 3). Six months after infection, people have stronger antibodies because the virus persists in the patient. The difference in antibody strength after infection and vaccination have not been compared. We should be careful to consider the differences between people with an effective versus an ineffective immune response against the virus.
Figure 3. Antibody maturation
After 6 months less antibody is required than after 1.3 months, indicating affinity maturation yielding stronger antibodies.
After 6 months less antibody is required than after 1.3 months, indicating affinity maturation yielding stronger antibodies.
Immune escape
Early in my scientific career I was involved in vaccine research on virus escape mutants. Escape mutants are variants of the virus that no longer bind to (group of) antibodies. This means that those antibodies became useless, but because a virus has mutated its epitopes. This becomes a problem if this happens for multiple epitopes. Mutations often lead to a 10- or 100-fold reduction in antibody binding strength. Antibodies that previously bound sufficiently could lose their binding capacity. In a similar fashion, viruses could also evade T-cell responses.
The virus escapes antibody-mediated neutralization by mutations. Half of the samples had lost all neutralizing activity. These viruses are therefore escape variants to which someone is again sensitive. Stronger antibodies still bind to mutated viruses after infection or after a second vaccination. A single virus escape mutant can also no longer be neutralized by the mature antibodies.
Escape variants are generated by the evolution of viruses (see example of evolution in the lab). Important for this process are:
The virus escapes antibody-mediated neutralization by mutations. Half of the samples had lost all neutralizing activity. These viruses are therefore escape variants to which someone is again sensitive. Stronger antibodies still bind to mutated viruses after infection or after a second vaccination. A single virus escape mutant can also no longer be neutralized by the mature antibodies.
Escape variants are generated by the evolution of viruses (see example of evolution in the lab). Important for this process are:
- High virus reproduction because many people are infected. With over 100 million infections worldwide a lot of mutations will be created. This will also increase the risk of recombination between mutants.
- Selection pressure by people with weak or partial immunity.
- Vaccination that is not 100% protected against infection, i.e., non-sterilizing immunity. Development of disease is irrelevant for virus evolution.
- People with a weak immune system.
- People who are reinfected after their immunity has waned.
Will immunity last?
Most but not all people are protected against the SARS-2 virus after infection or vaccination. It is estimated that after infection 5 to 10% are unprotected, comparable to the best vaccines. In the clinical studies, the Pfizer and Moderna mRNA vaccines protected extremely well against SARS-2 (90-95%). These vaccines work so well because they induce both CD4 and CD8 T cell responses.
The AstraZeneca adenovirus vector vaccine, which provides 60% protection, is likely to induce a mix of antibodies and T cells. It is realistic to expect that all vaccines will be slightly less effective in an uncontrolled setting because more vulnerable people will be vaccinated in real life than in clinical studies.
After infection, IgG antibodies against SARS-2 remain longer than five months (Figure 1). CD4 and CD8 T cells decrease by a factor of 3 and 5 over that time (Figure 4). 90% and 70% of patients have CD4 and CD8 at 1 to 2 months, and only 75% and 43% at 5 months. IgA decreases the most, 63% has this after 1 to 2 months after infection, but only 27% after five months. This means that sterilizing immunity, necessary for group immunity, only lasts for a short time in three quarters of people. We know that 5% of ex-patients have low immune responses after 6 months. Maybe these are the people who are reinfected.
Two important caveats to immunity should be noted. Follow-up is limited to 9 months or less. No studies investigate directly if people are protected only if they have immune responses against the virus.
The AstraZeneca adenovirus vector vaccine, which provides 60% protection, is likely to induce a mix of antibodies and T cells. It is realistic to expect that all vaccines will be slightly less effective in an uncontrolled setting because more vulnerable people will be vaccinated in real life than in clinical studies.
After infection, IgG antibodies against SARS-2 remain longer than five months (Figure 1). CD4 and CD8 T cells decrease by a factor of 3 and 5 over that time (Figure 4). 90% and 70% of patients have CD4 and CD8 at 1 to 2 months, and only 75% and 43% at 5 months. IgA decreases the most, 63% has this after 1 to 2 months after infection, but only 27% after five months. This means that sterilizing immunity, necessary for group immunity, only lasts for a short time in three quarters of people. We know that 5% of ex-patients have low immune responses after 6 months. Maybe these are the people who are reinfected.
Two important caveats to immunity should be noted. Follow-up is limited to 9 months or less. No studies investigate directly if people are protected only if they have immune responses against the virus.
Reinfection and persistent infection
Scientists distinguish reinfections and persistent infections. Persistence means that the virus is hiding somewhere in the body and may reappear in the sampled area, i.e., the nasal cavity. Reinfections can be positively identified when it is a different virus line. Persistent infections can be positively identified when virus persistence somewhere else in the body can be shown. Both mechanisms have been demonstrated, but in most cases, it is difficult to discriminate between these.
Some patients shed virus RNA for four months, e.g., some elderly people after mild infections. At high RNA concentrations, infectious virus can also be isolated despite neutralizing antibodies. This does not mean that this virus must be contagious, because virus surrounded by neutralizing antibodies might be easily eliminated by another person.
Some people suggest that RNA detected in RT-PCR is old RNA, but RNA has a stability of minutes not hours. For my thesis I detected RNA as viability marker of the tissue. All RNA will be digested by RNAse within 10 minutes at room temperature, and even shorter at body temperature. The suggestion of free RNA being detected in the body days or weeks after all virus being cleared, resembles Russel’s flying Teapot in an orbit around the sun.
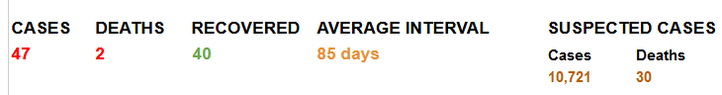
Corona common cold viruses reinfect people yearly. After about six months, antibody levels had decreased, the duration of T cell immunity is less well known. Cases of re-infection of SARS-2 have been described, both symptomatic after symptomatic and after asymptomatic. Re-infections can be severe or mild and follow a severe or milder infection. In 47 proven cases, it concerns two deaths:
Some patients shed virus RNA for four months, e.g., some elderly people after mild infections. At high RNA concentrations, infectious virus can also be isolated despite neutralizing antibodies. This does not mean that this virus must be contagious, because virus surrounded by neutralizing antibodies might be easily eliminated by another person.
Some people suggest that RNA detected in RT-PCR is old RNA, but RNA has a stability of minutes not hours. For my thesis I detected RNA as viability marker of the tissue. All RNA will be digested by RNAse within 10 minutes at room temperature, and even shorter at body temperature. The suggestion of free RNA being detected in the body days or weeks after all virus being cleared, resembles Russel’s flying Teapot in an orbit around the sun.
Corona common cold viruses reinfect people yearly. After about six months, antibody levels had decreased, the duration of T cell immunity is less well known. Cases of re-infection of SARS-2 have been described, both symptomatic after symptomatic and after asymptomatic. Re-infections can be severe or mild and follow a severe or milder infection. In 47 proven cases, it concerns two deaths:
- Twice first infection severe, second mild
- First infection serious, second serious
- Six times first mild (re) infection second is serious.
Sterilizing and herd immunity
Airway RNA viruses like influenza, RSV, corona- and rhinoviruses rarely induce sterilizing immunity. Sterilizing immunity means protection against disease and infection. Non-sterilizing immunity only protects against disease. These respiratory viruses manage to evade the immune system to spreading of the disease through asymptomatic people.
Most non-respiratory viruses cause sterilizing immunity. People with sterilizing immunity cannot be infected and therefore do not spread the virus further. This is a crucial step in the development of herd immunity. Some calculations:
If SARS-2 vaccination provides sterilizing immunity, the boundary formula for group immunity (HIT) is:
IgA is the antibody needed for sterilizing immunity, but only 78% of people produce IgA after infection. In addition, it appears that most of these only produce if during a short time - after three months all IgA has disappeared (Figure 6). IgG remains, so people do have antibodies and T cells to protect themselves against disease. Even van Dissel, the great Dutch advocate of herd immunity, no longer expected sterilizing immunity after vaccination.
Does non-sterilizing immunity always lead to less virus emissions? No, a study in influenza showed the opposite. Vaccinated people dispersed smaller droplets and spread more virus. The assumption that vaccination prevents contamination of respiratory viruses is dangerous and not based on scientific evidence. Infectiousness is a complex interaction between virus production and inflammatory response.
Studies in people after vaccination show the same picture for IgA production: short-time production during 2 - 3 months. In addition, type 1 interferon also helps in the first weeks after vaccination. So within three months after vaccination there is a temporary protective effect, which is very small for herd immunity and will disappears quickly again. Something similar was seen in Manaus when a lot of people were infected very quickly, the epidemic subsided for a while, and then continued at full speed.
Most non-respiratory viruses cause sterilizing immunity. People with sterilizing immunity cannot be infected and therefore do not spread the virus further. This is a crucial step in the development of herd immunity. Some calculations:
- If an average of ⅔ of the contacts of an infected person has sterilizing immunity, then an average of 1 - ⅔ = ⅓ of the people is susceptible to the virus.
- If someone has an average of 3 contacts (R0 = 3, basic reproduction number) then the effective reproduction is (Re) = ⅓ * 3 = 1. That is the point at which the contamination does not increase or decrease further.
- When Re ~ 1, the epidemic rate decreases to the status quo and not the exponential function. So scientist could easily monitor that herd immunity has almost been reached.
If SARS-2 vaccination provides sterilizing immunity, the boundary formula for group immunity (HIT) is:
- I * Si> = 1 - 1 / R0
- R0 = reproduction number
- I =% of people who are immune (90-95%).
- Si =% of people with sterilizing immunity in the immune group.
IgA is the antibody needed for sterilizing immunity, but only 78% of people produce IgA after infection. In addition, it appears that most of these only produce if during a short time - after three months all IgA has disappeared (Figure 6). IgG remains, so people do have antibodies and T cells to protect themselves against disease. Even van Dissel, the great Dutch advocate of herd immunity, no longer expected sterilizing immunity after vaccination.
Does non-sterilizing immunity always lead to less virus emissions? No, a study in influenza showed the opposite. Vaccinated people dispersed smaller droplets and spread more virus. The assumption that vaccination prevents contamination of respiratory viruses is dangerous and not based on scientific evidence. Infectiousness is a complex interaction between virus production and inflammatory response.
Studies in people after vaccination show the same picture for IgA production: short-time production during 2 - 3 months. In addition, type 1 interferon also helps in the first weeks after vaccination. So within three months after vaccination there is a temporary protective effect, which is very small for herd immunity and will disappears quickly again. Something similar was seen in Manaus when a lot of people were infected very quickly, the epidemic subsided for a while, and then continued at full speed.
Figure 6. Course of IgM, IgG and IgA antibodies from the onset of symptoms
New vaccines for sterilizing immunity
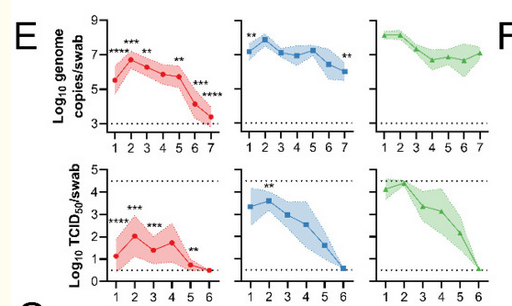
The primary aim of vaccination is to protect against disease, but herd immunity could be a nice and desirable side effect of vaccination. This would allow unvaccinated people to have some protection as well, which is also a good sales argument for pharmaceutical companies. The current SARS-2 vaccines induce T cells and IgG to preventing disease. Without IgA, it is unlikely that immunity would be sterilizing. Most respiratory infection vaccines provide only limited protection against virus replication in the upper respiratory tract, as this requires an IgA in the mucosa. A lot of vaccination research has been performed to investigate which kind of vaccines induced IgA. Intranasal vaccination could be suitable, especially with adenovector vaccine. These are being developed in China, India, and the USA. A study with the AstraZeneca vaccine in hamsters shows that vaccination in the nose and in the muscles leads to antibodies in the circulation (Figure 7), but only intranasal vaccination produces sterilizing immunity (Figure 8).
Figure 7. Virus neutralization after vaccination
Figure 8. Virus titers after infection in hamsters vaccinated with the AstraZeneca vaccine AZD1222 in the nose (red) or muscle (blue) and control (green). The top line is for RNA copies, the bottom line for infectious virus.
Unethically acts.
Now I will return to the ethical principles of the Dutch policies. The good thing the Netherlands strife for suggests that the lives of some people are more valuable than those of others.
The Netherlands broke with European ethical principles that required to vaccinate vulnerable people first. The Dutch are making an unjustified appeal to herd immunity. Healthcare workers would be much better protected from appropriate facemasks, which still fall short for many care workers. Shifting to herd immunity lacks scientific basis and is violates ethical guidelines of the European Medicines Authority (EMA) and the Dutch Health Council. In an ultimate attempt to stop the government, the Health Council repeated the same advice another three times. Politicians may repeat themselves a lot, but scientists generally just let the evidence speak.
I am a scientist and I also repeat my message. I started with the allowance gate to illustrate the ethical limits of a democracy. I would recommend a parliamentary inquiry for both the allowance gate and the Covid policies. Not only the vaccination, but several decisions in this epidemic raised doubt about the separation of science and politics in integrity and epidemic control.
The Netherlands broke with European ethical principles that required to vaccinate vulnerable people first. The Dutch are making an unjustified appeal to herd immunity. Healthcare workers would be much better protected from appropriate facemasks, which still fall short for many care workers. Shifting to herd immunity lacks scientific basis and is violates ethical guidelines of the European Medicines Authority (EMA) and the Dutch Health Council. In an ultimate attempt to stop the government, the Health Council repeated the same advice another three times. Politicians may repeat themselves a lot, but scientists generally just let the evidence speak.
I am a scientist and I also repeat my message. I started with the allowance gate to illustrate the ethical limits of a democracy. I would recommend a parliamentary inquiry for both the allowance gate and the Covid policies. Not only the vaccination, but several decisions in this epidemic raised doubt about the separation of science and politics in integrity and epidemic control.
John Jacobs
24.02.2021
24.02.2021