COVID-19
Excess mortality in Europe |
1. Key points
- Covid has caused a stable excess mortality all over Europe of 10-12% in 2022.
- North, South and East Europe were hit hard, harder, and hardest, respectively; Most countries follow regional trends.
- Mitigation strategies like reducing transmission and vaccination seemed to be about equally effective.
- South and East-European countries were hit hardest in 2020, possibly due to being hit first.
- East-European countries were hit harder in 2021, possibly related to delayed vaccination and reduced mitigation.
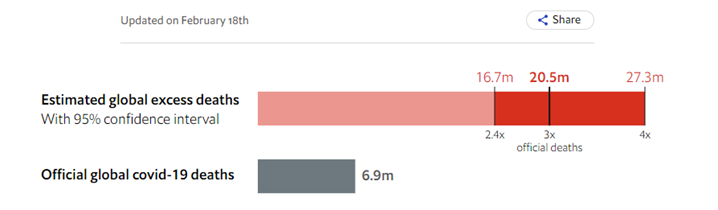
- World-wide inequities in healthcare will be larger in low-income countries.
- The Netherlands was hit harder than other countries in North-and even South-Europe, due to a deliberately chosen different epidemic coping strategy.
2. Analysis of excess mortality
Previous analytics has shown that different areas in Europe had different levels of COVID-19 related mortality. Because of the reported unreliability of covid-mortality, this paper uses excess mortality. Countries of the European Economic Area (EEA) with at least 4 million people were grouped in three regions:
Full methods can be found in the Supplement EM
- East: Bulgaria, Croatia, Czechia, Greece, Hungary, Poland, Romania, Slovakia, and Slovenia.
- North: Belgium, Denmark, Finland, Germany, Ireland, Netherlands, Norway, and Sweden.
- South: Austria, France, Italy, Portugal, Spain, and Switzerland.
Full methods can be found in the Supplement EM
3. Excess mortality in European regions
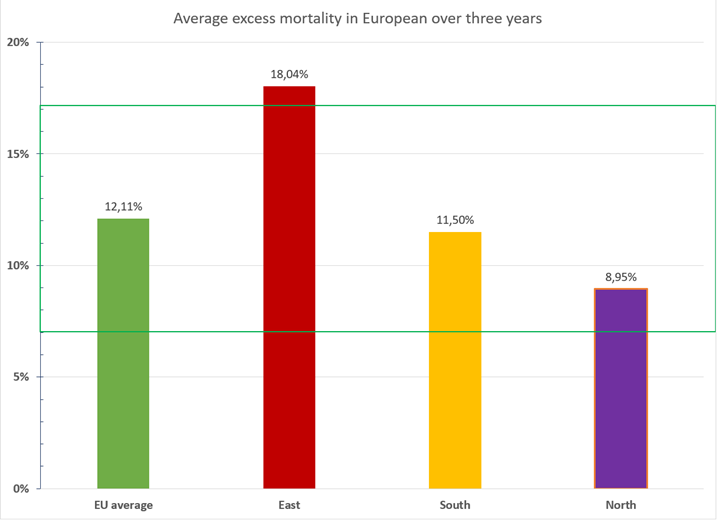
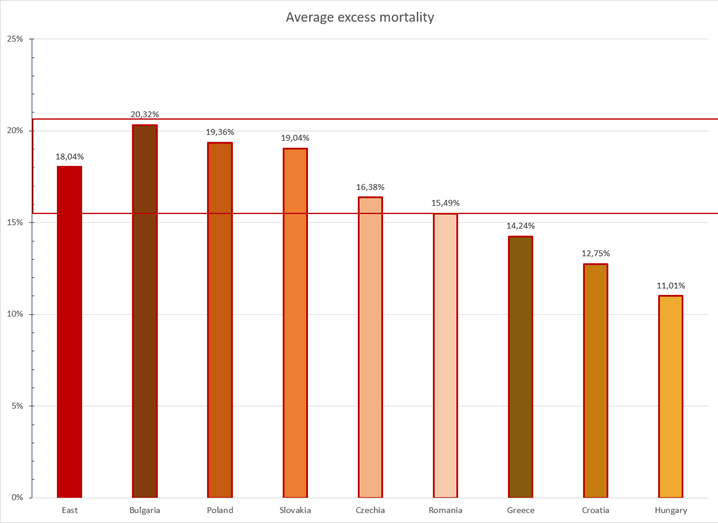
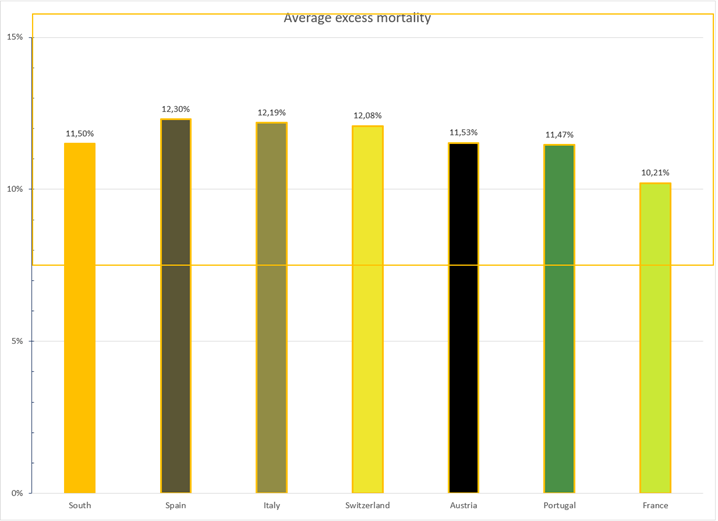
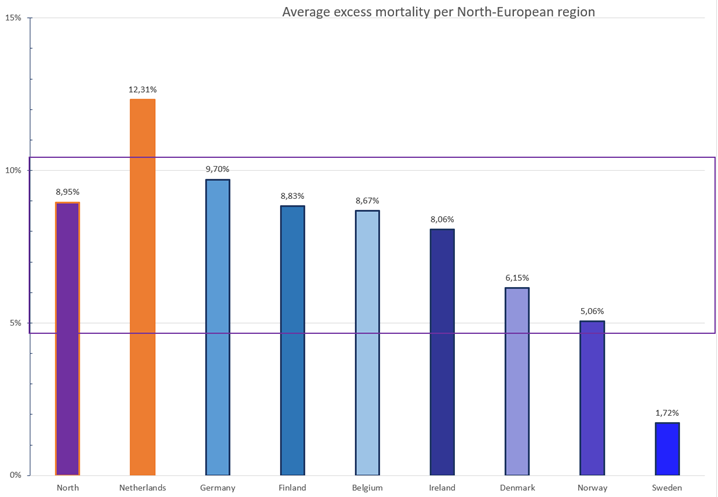
Three years of COVID-19 epidemics have led to over 12% excess mortality all over the EEA (Figure 1). Excess mortality in East-, South-, and North-European countries was 18%, 12% and 9%, respectively.
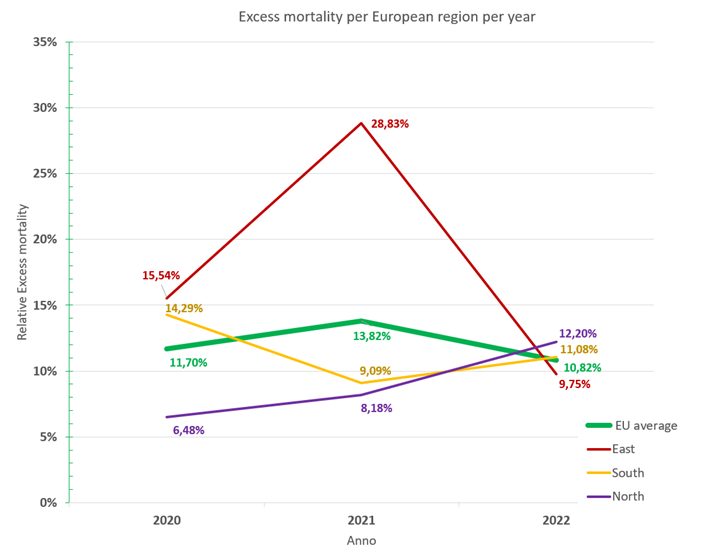
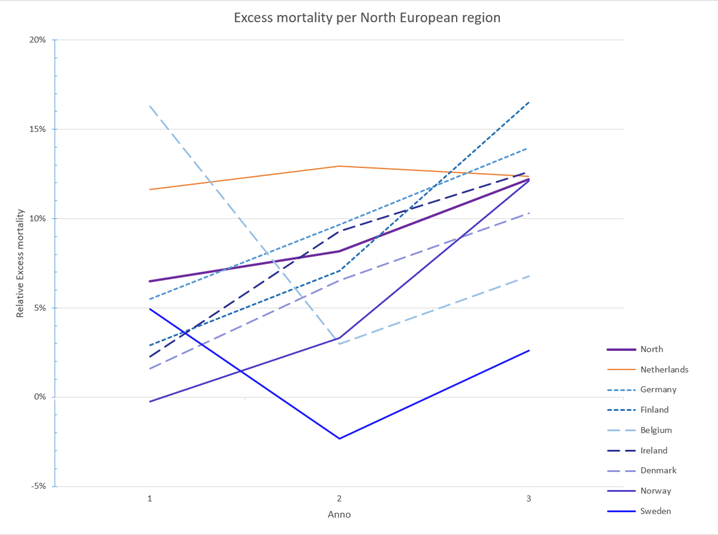
Focusing on results per year show that the North-European countries were hit less hard in 2020 with only 6% excess mortality, compared to 14% and 16% for South and Europe (Figure 2). In the beginning of the epidemic, South-European countries were the first ones to be hit by surprise, resulting in excess mortality.
In 2021, when containment was relaxed and vaccination started rollout started, excess mortality slightly increased to 8% for North, decreased to 9% for South, but increased to 29% for East-Europe. The difference in 2021 might be partly due to delayed rollout of vaccination in East-Europe (see Supplement EM).
In 2022, all European regions seem to be close together between 10% and 12 % excess mortality.
In 2020, prevention of virus spreading seem to be the most important mitigation, in 2022, this was replaced by vaccination. Both have a similar efficacy. The high excess mortality rates in some East-European countries in 2021 hint to what the impact would be without a mitigation strategy.
The European Union has supported the equal distribution of vaccines over its member states. Inequity differences are expected to be much higher in other areas of the world, like South America, Africa, and Asia. Reliable data for comparison is lacking from these countries.
Focusing on results per year show that the North-European countries were hit less hard in 2020 with only 6% excess mortality, compared to 14% and 16% for South and Europe (Figure 2). In the beginning of the epidemic, South-European countries were the first ones to be hit by surprise, resulting in excess mortality.
In 2021, when containment was relaxed and vaccination started rollout started, excess mortality slightly increased to 8% for North, decreased to 9% for South, but increased to 29% for East-Europe. The difference in 2021 might be partly due to delayed rollout of vaccination in East-Europe (see Supplement EM).
In 2022, all European regions seem to be close together between 10% and 12 % excess mortality.
In 2020, prevention of virus spreading seem to be the most important mitigation, in 2022, this was replaced by vaccination. Both have a similar efficacy. The high excess mortality rates in some East-European countries in 2021 hint to what the impact would be without a mitigation strategy.
The European Union has supported the equal distribution of vaccines over its member states. Inequity differences are expected to be much higher in other areas of the world, like South America, Africa, and Asia. Reliable data for comparison is lacking from these countries.
Figure 1. Average excess mortality per European region over three years. The green box indicates the SD for EU average.
Figure 2. Excess mortality per European region per year
4. Most countries follow regional trends.
The average excess mortality rates of most countries neatly fit their respectively regions, with the mortality rates in East-, South-, and North-Europe, being, 11 to 20%, 10 to 12%, and 2 to 12% respectively (Figure 3; Figure 4; Figure 5).
Two countries have an excess mortality rate that would better fit in another region.
First, Hungary (Figure 3) has lower mortality than other East-European countries and would fit better in the group of South-European countries, where its neighbouring country Austria is grouped (Figure 4).
The other is the Netherlands (Figure 5). Although located in between North-European countries only, it has the highest excess mortality from the North-European region, scoring even higher than all south-European counties and Hungary.
Sweden had the lowest mortality rates of all countries. At the start of the epidemic, Sweden had the highest mortality rates in Scandinavia, but then Sweden changed it strategy from herd immunity to responsible containment. In the second and third year this led to lower excess mortality (Figure 6)..
Two countries have an excess mortality rate that would better fit in another region.
First, Hungary (Figure 3) has lower mortality than other East-European countries and would fit better in the group of South-European countries, where its neighbouring country Austria is grouped (Figure 4).
The other is the Netherlands (Figure 5). Although located in between North-European countries only, it has the highest excess mortality from the North-European region, scoring even higher than all south-European counties and Hungary.
Sweden had the lowest mortality rates of all countries. At the start of the epidemic, Sweden had the highest mortality rates in Scandinavia, but then Sweden changed it strategy from herd immunity to responsible containment. In the second and third year this led to lower excess mortality (Figure 6)..
Figure 3. Excess mortality East-European countries. The orange box indicates the SD for East European countries.
Figure 4. Excess mortality South European countries. The yellow box indicates the SD for South-Europe.
Figure 5. Excess mortality North-European countries. The purple box indicates the SD for North European countries.
5. Excess mortality in the Netherlands
The only remarkable exception to the rule that most countries fit their regional tendency are the Netherlands. The high excess mortality rate in the Netherlands compared to its neighbour was seen in every year of the epidemic (Figure 6). This could not be explained topographically, since the Netherlands are embedded in between North-European countries. The Netherlands have even a higher score even than all South-European countries, while all other North-European countries have lower scores.
What could be the cause of the elevated excess mortality in Netherlands?
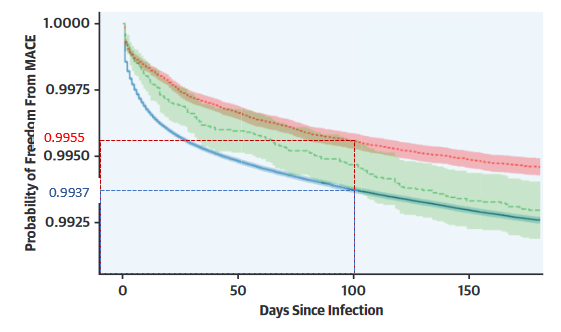
Vaccination cannot be linked to unexpected deaths and is associated with decreased mortality e.g., by reduced numbers of lethal cardiovascular events (Figure 7a). The vaccination grade in the Netherlands is only marginally lower than in most other countries in North and South Europe, so this could not explain the observed increased excess mortality.
The Netherlands has a long history of ignoring[iv] international health advice on the Covid-19 epidemic. Testing & isolating was never an important part of its anti-epidemic strategy. The Netherlands focused on testing of symptomatic people for medical reasons, ignoring that people have the highest virus titers before or without having symptoms.
The policy drive[viii] in the Netherlands was based on a different ideology. Its strategy aims for herd immunity through natural infection, with focus on how much immunity was gained in the population by infection and vaccination.
Recently, the Netherlands have opted for the next step in covid epidemiology: completely ignoring the epidemiology of this pathogen. In other words, the country will continue its strategy. Related to higher excess mortality will also be a higher incidence of long covid in the Netherlands, as well as higher costs for health care and higher economic loss associated with increased disease incidence.
What could be the cause of the elevated excess mortality in Netherlands?
Vaccination cannot be linked to unexpected deaths and is associated with decreased mortality e.g., by reduced numbers of lethal cardiovascular events (Figure 7a). The vaccination grade in the Netherlands is only marginally lower than in most other countries in North and South Europe, so this could not explain the observed increased excess mortality.
The Netherlands has a long history of ignoring[iv] international health advice on the Covid-19 epidemic. Testing & isolating was never an important part of its anti-epidemic strategy. The Netherlands focused on testing of symptomatic people for medical reasons, ignoring that people have the highest virus titers before or without having symptoms.
The policy drive[viii] in the Netherlands was based on a different ideology. Its strategy aims for herd immunity through natural infection, with focus on how much immunity was gained in the population by infection and vaccination.
Recently, the Netherlands have opted for the next step in covid epidemiology: completely ignoring the epidemiology of this pathogen. In other words, the country will continue its strategy. Related to higher excess mortality will also be a higher incidence of long covid in the Netherlands, as well as higher costs for health care and higher economic loss associated with increased disease incidence.
Figure 6. Yearly excess mortality in North Europe.
Figure 7a. Risk cardiovascular event 100 dags after COVID-19 is 4.5 / 1000 for fully vaccinated and 7.3 / 1000 for unvaccinated.
6. Conclusion
Regional factors might have a large influence on excess mortality, as these might be related to virus spread and abilities to counteract this. Allowing more infections implies more disease, more mortality, more long-covid disease, and more economic costs. Protection from epidemic is a human right and a combination of measures might be required. Ethical concerns can be raised for the Dutch covid policies, the wording unethical and unscientific have been used by the World Health Organization (WHO). Stupidity rules if we want to become infected, so that we will be protected from infection (Figure 7).
Methods and additional data can be found in the supplement EM.
Methods and additional data can be found in the supplement EM.
Figuur 7b. Logica van immuniteit door infectie
John Jacobs
25.02.20223
25.02.20223