COVID-19The disease and long-term effectsJohn Jacobs
|
Lethal for vulnerable people
SARS-2 is not a major killer, but has a much higher infection fatality rate than influenza (0.04-0.1%). Ir estimated in the early days a mortality rate of 0.6 to 2.9%, but now I would estimate the lower part of this only: 0.6 to 1%. This is a much higher rate than even a severe flu. The lockdown reduced the number of infection to about 6% of the Dutch population. The yielded excess mortality of 10.000 on a population of 17 million could thus raise to more than 100.000 if everyone would be infected. We should not only fight this epidemic because of mortality rates, also morbidity and prolonged disease are serious consequences of COVID-19.
Different symptoms
Like most respiratory viruses, SARS-2 infections could result in very different symptoms for different patients (Zimmer). Some people have barely symptoms. Other will have fever, shortage of breath, coughing and sneezing. Some people will need hospital or intensive-care treatment for weeks. COVID-19 can affect the lungs and immune system and can even lead to strokes and psychosis. Breathing problems and post-viral fatigue can last for months in some cases (Clip BBC).
Long COVID
Long COVID means that people, often after a mild disease, have prolonged symptoms (Spencer). This phenomenon is known from many other viruses, including the related coronaviruses SARS-1 and MERS. One year after SARS-1, 24% of the former patients had a clearly decreased condition (Hui). The lung function was still reduced in over 50% of the former patients, two years after the disease (Ngai).
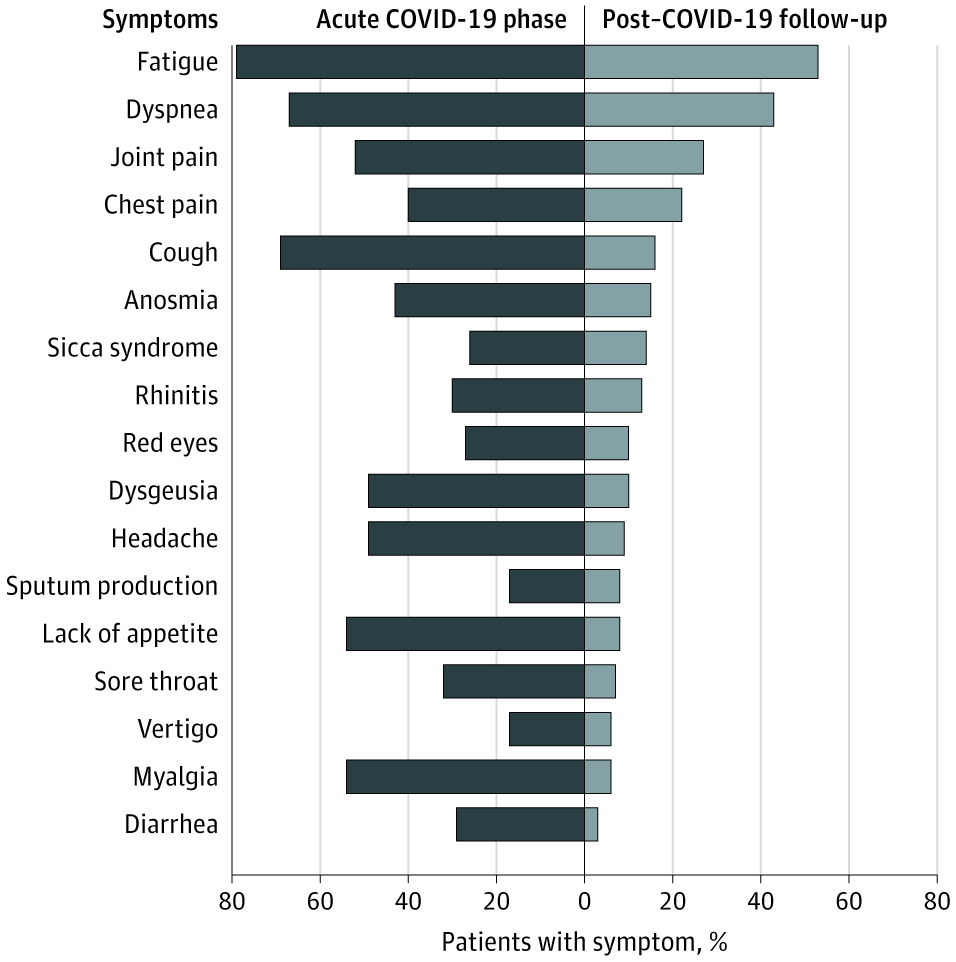
Most patients are not completely recovered, two months after COVID-19 (Carfì). The BMJ made a webinar on long COVID. The symptoms vary strongly from person to person, and even from day to day in some persons, being extremely tired on one day, while having barely complaints the next day. Fatigue, dyspnoea, joint and chest pain are high on the list of symptoms (Figure 1). These symptoms and cardiac disease (not measure here) could also arise in young and healtht patients who had no or only mild disease (Barber).
Most patients are not completely recovered, two months after COVID-19 (Carfì). The BMJ made a webinar on long COVID. The symptoms vary strongly from person to person, and even from day to day in some persons, being extremely tired on one day, while having barely complaints the next day. Fatigue, dyspnoea, joint and chest pain are high on the list of symptoms (Figure 1). These symptoms and cardiac disease (not measure here) could also arise in young and healtht patients who had no or only mild disease (Barber).
Figure 1. Symptoms during and two months after COVID-19 (Carfì).
Pathological strong defences
It is clear that a strong, but inadequate, immune response against SARS-2 yields COVID-19. COVID-19 is a multisystem inflammatory syndrome with immunological responses throughout the body. The symptoms of long COVID are independent of risk groups and severity of the disease course. Children who have had asymptomatic SARS-2 infection can also suffer serious heart damage. A total of 662 children have been described with this disease, including 11 fatal cases (Sciencedaily).
The strong immune reaction causes the disease, but it is not clear how. Some researchers blame a cytokine storm, but others point to the much lower concentrations of cytokines in COVID-19 (Kox). Possibly could antibody-mediated virus dissemination cause multiple local infections with immunological damage (Jacobs).
The strong immune reaction causes the disease, but it is not clear how. Some researchers blame a cytokine storm, but others point to the much lower concentrations of cytokines in COVID-19 (Kox). Possibly could antibody-mediated virus dissemination cause multiple local infections with immunological damage (Jacobs).
long-term disease
The long-term symptoms of COVID-19 are not clear. Chronic COVID-19 symptoms are a serious problem for a considerable group of patients, with mild or sever COVID-19. The estimates vary and the numbers decrease in time. Numbers could be around 20% after 3 months, and halve of this after 6 months. Systematic research into long COVID should be performed
John Jacobs
12 - 09 - 2020
12 - 09 - 2020