COVID-19
Beyond mortality
John Jacobs, 6th March 2021.
Short-term mortality rates underestimate the impact of COVID-19. SARS-2 infections cause serious morbidity as well, including chronic disease. Morbidity is more difficult to calculate, so physicians use Quality-Adjusted Life Years (QALYs), in which loss of quality of life and longevity are combined. In the epidemics of SARS-1 and MERS, but also influenza, the loss in QALYs was mainly due to the mortality rates. In SARS-2, long-term and chronic illness seem to be the major contribution to the loss of QALYs.
The life expectancy of some people after an acute SARS-2 infection could be reduced by ten years due to the chronic diseases caused by SARS-2. Others may be more susceptible to mortality due to (SARS-2) reinfections or have relevant loss of quality of life. Therefore, after discussing the mortality rates, I will also address long-term illness and lasting effects of SARS-2. From an mechanistical point of view, immunology seems to be crucial in SARS-2 infection, related to the strong but ineffective immune response it evokes.
The life expectancy of some people after an acute SARS-2 infection could be reduced by ten years due to the chronic diseases caused by SARS-2. Others may be more susceptible to mortality due to (SARS-2) reinfections or have relevant loss of quality of life. Therefore, after discussing the mortality rates, I will also address long-term illness and lasting effects of SARS-2. From an mechanistical point of view, immunology seems to be crucial in SARS-2 infection, related to the strong but ineffective immune response it evokes.
Mortality rates
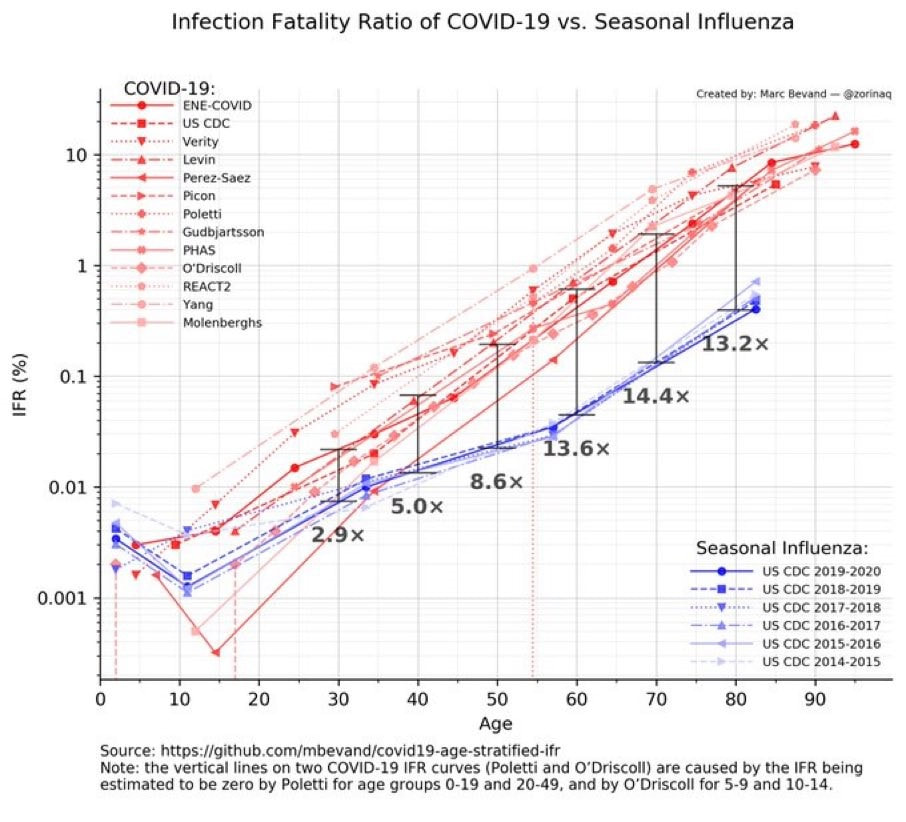
Mortality rates after virus infections should be compared by infection-fatality ratios (IFRs), i.e., percentage of lethal cases after infection. However, the IFR is not available for many diseases, because in general we do not monitor how many people were infected. Often the case-fatality ratio (CFR) is calculated, the lethal percentage of people who got disease. It is crucial to understand that many people do not get sick after any virus infection. This is exemplified in the annual flu wave, where only a small percentage get influenza. In case of a SARS-2 infection, about half will become ill, but limited data are available. Thus, the CFR is about twice as high as the IFR. For influenza, the difference between IFR and CFR is much larger, but not known precisely. This hinders a good approximation of the IFR for influenza.
Although influenza is subject of intensive research, the data on influenza infections is very limited, in general only cases are recorded. When the IFR can be calculated, SARS-2 is about 10 times more as lethal than influenza, with differences between age groups (Figure 1). If 50% of the population would be infected during an influenza epidemic – the point of herd immunity without mitigation - the IFR of a serious influenza epidemic would be a factor of 25 lower than the current CFR-based estimate. Thus SARS-2 maybe 250 times as lethal than the flu.
Although influenza is subject of intensive research, the data on influenza infections is very limited, in general only cases are recorded. When the IFR can be calculated, SARS-2 is about 10 times more as lethal than influenza, with differences between age groups (Figure 1). If 50% of the population would be infected during an influenza epidemic – the point of herd immunity without mitigation - the IFR of a serious influenza epidemic would be a factor of 25 lower than the current CFR-based estimate. Thus SARS-2 maybe 250 times as lethal than the flu.
Figure 1. IFR of COVID-19 compared to influenza.
The IFR of influenza assumes a low infection percentage in the population, which means that the IFR may be too high by a factor of 5 to 50
The IFR of influenza assumes a low infection percentage in the population, which means that the IFR may be too high by a factor of 5 to 50
Relative risks
Age is an important predictor of the infection fatality risk for many diseases. For influenza, the difference is 100-fold between young and old, divided into a factor of 10 between 20 and 55 and between 55 and 80 years old. SARS-2 has a factor of 1000 between young and old: factor 10 between 15 and 40, 40 and 60, 60 and 80 years old. People from 30 and 60 years old have a 3- and 14-fold increased risk to die from SARS-2 compared to influenza. Prior to the rise of the British mutant, young children had a similar risk of dying due to influenza compared to SARS02. In the Netherlands, the average IFR was just above 0.9% in the first wave and just below 0.9% in the second wave.[1] The slightly lower mortality rate is not due to improvement of the therapy, but mainly to self-quarantine of vulnerable people. In Germany, the IFR is 1.1%. Depending on the population, the IFR may be slightly higher or lower in different countries.
Untreated diabetes, cardiovascular disease, and obesity are other important risk factors for lethal SARS-2. Men have a greater risk than women, possibly because of stronger immune reactions. Genetic "defects", such as reduced production of type 1 interferon that is normally undetected, are also an important risk-increasing factor. Apparently healthy young people who produce less type 1 interferon can die from SARS-2. It is therefore not the case that everyone knows that he or she is at increased risk.
[1] The excess mortality in the 2nd wave is almost 9,000 people, together with the more than 10,000 deaths from the first wave, that is 19,000 deaths. According to Sanquin, 13% of the 17.15 million Dutch people are infected. This gives an IFR of 0.88%.
Untreated diabetes, cardiovascular disease, and obesity are other important risk factors for lethal SARS-2. Men have a greater risk than women, possibly because of stronger immune reactions. Genetic "defects", such as reduced production of type 1 interferon that is normally undetected, are also an important risk-increasing factor. Apparently healthy young people who produce less type 1 interferon can die from SARS-2. It is therefore not the case that everyone knows that he or she is at increased risk.
[1] The excess mortality in the 2nd wave is almost 9,000 people, together with the more than 10,000 deaths from the first wave, that is 19,000 deaths. According to Sanquin, 13% of the 17.15 million Dutch people are infected. This gives an IFR of 0.88%.
Infection
Just like many respiratory infections, symptomatic SARS-2 starts with the initiation of the immune response against the virus. Not everyone will have symptoms after infection, only people whose immune system is inefficient in eliminating the virus. In case of SARS-2, this is about half of the people infected. In addition to spreading the virus from one tissue to another, most of the symptoms appear to be independent of each other. The virus mainly infects cells with ACE2.
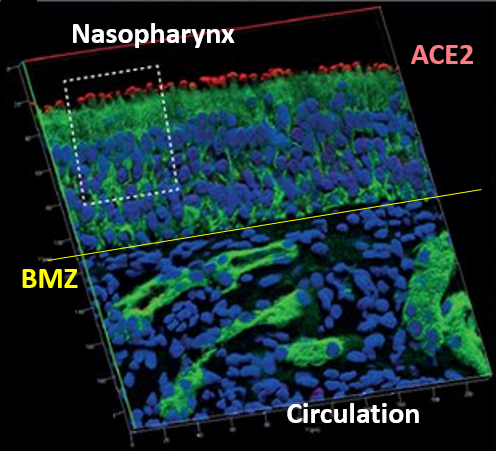
These cells are important in almost every organ, including the lungs, brain, intestines, and smooth muscle around slightly larger blood vessels, and regulate blood flow for organs. More ACE2 is found in the nasal epithelium than in the lungs and the highest concentration is on the nasal cavity side of this epithelium, separated from the blood circulation by the basement membrane (Figure 2). The nasal epithelium also contains nerve processes that have connections to the brain, but they do not have ACE2. Still, some researchers think that the SARS-2 virus can also enter the brain via this route, but other routes are also possible.
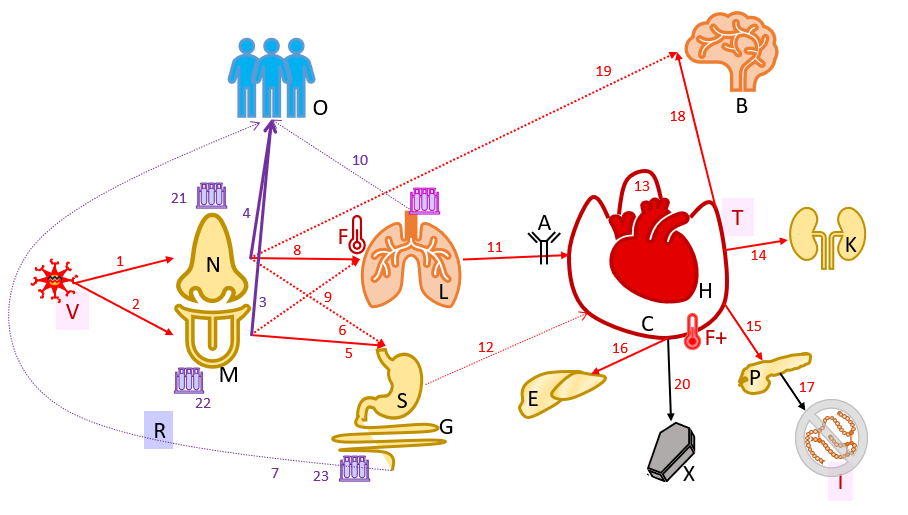
Virus infection starts at the nose and oral cavity (Figure 3). Loss of smell and taste is the first specific symptom of SARS-2 infection, which occurs in 85% of symptomatic people. The virus can spread to other people after local multiplication in the nasal cavity. These infected people are still presymptomatic and the virus is still shielded from the circulation. The innate immune system can defeat the virus by actions of type 1 interferons and other factors, avoiding symptomatic disease. Like other respiratory viruses, most of the virus is produced in humans just before and a few days after the onset of symptoms. In this phase all people are without complaints, so asymptomatic. Some infected people develop symptoms later and were thus presymptomatic, others never develop symptoms and are therefore true asymptomatic.
The virus can spread from the upper respiratory tract to the gastrointestinal tract and lungs. There the specific immune system is activated and a fever and severe pneumonia - Severe Acute Respiratory Syndrome (SARS) – will develop. Gastrointestinal infection could alter the intestinal flora by decreasing harmless bacteria and increasing pathogens.
From the lungs or the intestines, the virus could spread to the blood circulation. Via the circulation, the virus can cause infection and damage in all organs, but also thrombosis and general inflammatory mechanisms such as high fever. The disease could affect the brain, liver, kidneys, and pancreas, but tissue damage can also occur in various organs. Brain fog is a well-known symptom that could last for months after disease. In the pancreas, insulin-producing cells could be destroyed, leading todiabetes. SARS-2 infection could elevate liver enzymes and also cause kidney failure.
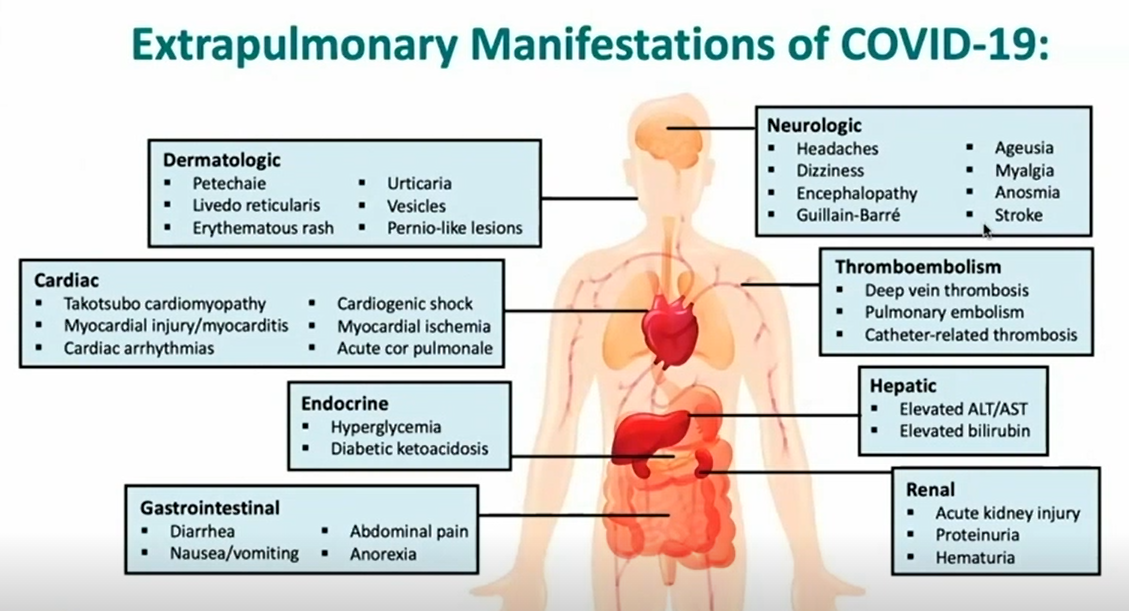
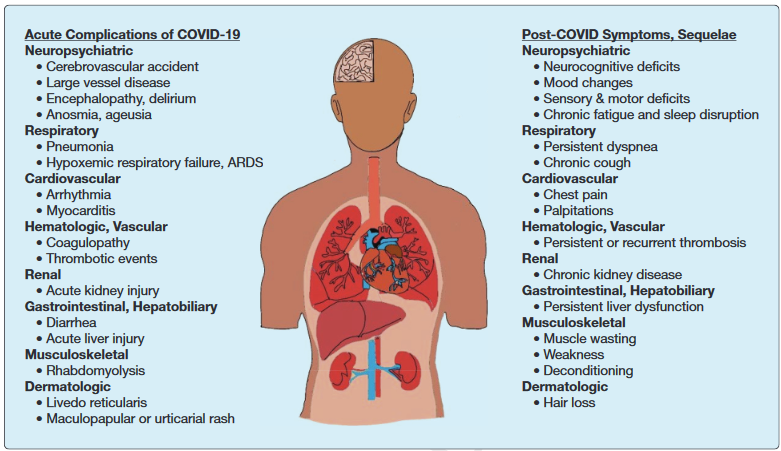
Corona infections are often but not always limited to the respiratory tract. In case of SARS-2, many people have symptoms all through the body, including the gastrointestinal tract, circulation, heart, kidneys, liver, pancreas, brain, and skin (Figure 4).
These cells are important in almost every organ, including the lungs, brain, intestines, and smooth muscle around slightly larger blood vessels, and regulate blood flow for organs. More ACE2 is found in the nasal epithelium than in the lungs and the highest concentration is on the nasal cavity side of this epithelium, separated from the blood circulation by the basement membrane (Figure 2). The nasal epithelium also contains nerve processes that have connections to the brain, but they do not have ACE2. Still, some researchers think that the SARS-2 virus can also enter the brain via this route, but other routes are also possible.
Virus infection starts at the nose and oral cavity (Figure 3). Loss of smell and taste is the first specific symptom of SARS-2 infection, which occurs in 85% of symptomatic people. The virus can spread to other people after local multiplication in the nasal cavity. These infected people are still presymptomatic and the virus is still shielded from the circulation. The innate immune system can defeat the virus by actions of type 1 interferons and other factors, avoiding symptomatic disease. Like other respiratory viruses, most of the virus is produced in humans just before and a few days after the onset of symptoms. In this phase all people are without complaints, so asymptomatic. Some infected people develop symptoms later and were thus presymptomatic, others never develop symptoms and are therefore true asymptomatic.
The virus can spread from the upper respiratory tract to the gastrointestinal tract and lungs. There the specific immune system is activated and a fever and severe pneumonia - Severe Acute Respiratory Syndrome (SARS) – will develop. Gastrointestinal infection could alter the intestinal flora by decreasing harmless bacteria and increasing pathogens.
From the lungs or the intestines, the virus could spread to the blood circulation. Via the circulation, the virus can cause infection and damage in all organs, but also thrombosis and general inflammatory mechanisms such as high fever. The disease could affect the brain, liver, kidneys, and pancreas, but tissue damage can also occur in various organs. Brain fog is a well-known symptom that could last for months after disease. In the pancreas, insulin-producing cells could be destroyed, leading todiabetes. SARS-2 infection could elevate liver enzymes and also cause kidney failure.
Corona infections are often but not always limited to the respiratory tract. In case of SARS-2, many people have symptoms all through the body, including the gastrointestinal tract, circulation, heart, kidneys, liver, pancreas, brain, and skin (Figure 4).
Figure 3. The course of SARS-2 infection.
Red lines indicate the spread of the virus, green lines detection, black lines other processes. Dashed lines are possible routes that are rarely used. B = Brain; C = blood Circulation; E = Liver, F = fever, F + = high fever, G = Intestinal system; H = Heart; I = Insulin; K = Kidneys; L = Lungs; M = Oral cavity; N = Nose; O = other people, P = pancreas; R = RT-CPR (RNA detection); S = Stomach; T = Thrombosis; V = SARS-2 virus. SARS-2 [V] infects the epithelium of (1) the nose [N] and (2) the mouth [M]. These (3,4) are probably the most important routes for infecting other people and start before anyone has symptoms. The gastrointestinal tract [S, G] is also infected from (5) the mouth and (6) the nose. In theory, (7) the stool could be a source of contamination for other people [O]. From the nose and throat (8,9) the lungs are infected, the lung disease can lead to (F) fever. The virus from the lungs [L] (10) could also infect others. Probably from (11) the lungs, but from (12) the gastrointestinal tract it is possible for the virus to enter the circulation [C]. This is the time when the antibody reaction starts in a normal infection. Via the circulation, the (13) heart [H], (14) the kidneys [K], (15) the pancreas [P], (16) the liver {E] can be infected. Damage can occur in all these organs, in the pancreas (17) this can lead to diabetes [I]. The brain [B] can also be infected from the circulation (18) or possibly directly from nerves in the nose (19). The violent immune response against SARS-2 leads to an increase in fever [F +] and thrombosis [F], the latter with possible damage in all organs. At (20) a small group to death [X]. The virus can be isolated at different times from (21) the nose, (22) the oral cavity, and (23) the stool
Red lines indicate the spread of the virus, green lines detection, black lines other processes. Dashed lines are possible routes that are rarely used. B = Brain; C = blood Circulation; E = Liver, F = fever, F + = high fever, G = Intestinal system; H = Heart; I = Insulin; K = Kidneys; L = Lungs; M = Oral cavity; N = Nose; O = other people, P = pancreas; R = RT-CPR (RNA detection); S = Stomach; T = Thrombosis; V = SARS-2 virus. SARS-2 [V] infects the epithelium of (1) the nose [N] and (2) the mouth [M]. These (3,4) are probably the most important routes for infecting other people and start before anyone has symptoms. The gastrointestinal tract [S, G] is also infected from (5) the mouth and (6) the nose. In theory, (7) the stool could be a source of contamination for other people [O]. From the nose and throat (8,9) the lungs are infected, the lung disease can lead to (F) fever. The virus from the lungs [L] (10) could also infect others. Probably from (11) the lungs, but from (12) the gastrointestinal tract it is possible for the virus to enter the circulation [C]. This is the time when the antibody reaction starts in a normal infection. Via the circulation, the (13) heart [H], (14) the kidneys [K], (15) the pancreas [P], (16) the liver {E] can be infected. Damage can occur in all these organs, in the pancreas (17) this can lead to diabetes [I]. The brain [B] can also be infected from the circulation (18) or possibly directly from nerves in the nose (19). The violent immune response against SARS-2 leads to an increase in fever [F +] and thrombosis [F], the latter with possible damage in all organs. At (20) a small group to death [X]. The virus can be isolated at different times from (21) the nose, (22) the oral cavity, and (23) the stool
Figure 4. Extrapulmonary SARS-2 symptom
Beyond acute disease
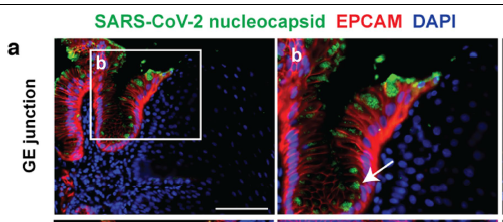
Usually, the virus is first cleared in the upper respiratory tract and then in the lungs. This implies that nasopharyngeal swabs for routine RT-PCR test fail to sample the virus, but that the patient still is infected. People with negative or extremely low RT-PCR titers are unlikely to be infectious, but this does not imply that these have recovered from disease. After the virus clearance in the lungs, it could still a long time to recover from disease. Often, the symptoms of lung disease exacerbate in the months after infection. In some people, the virus remains in the intestines for many months. The recurrence of airway infection by the same strain suggests persistent infection elsewhere in the body. Recent research shows virus particles in the gut three months after the onset of infection (Figure 5). In the recovery phase, the complaints due to COVID-19 can still increase (see “Afterburner”).
Figure 5. Virus particles (green) in the intestinal epithelium, three months after infection onset in "cured" COVID-19 patients
Lung disease
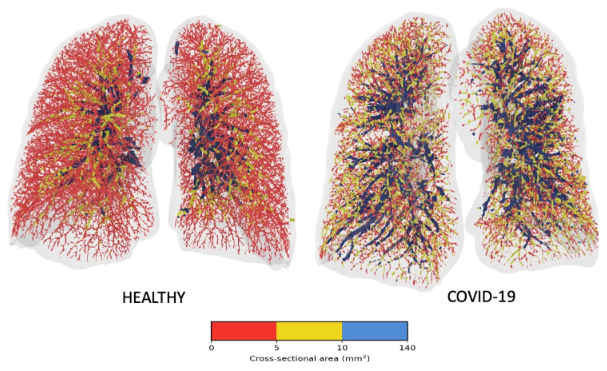
Medical scientists could not match the blood oxygen concentrations with the relatively limited pneumonia. In the lungs, the ACE2 molecule is mainly located on the small blood vessels to be involved in the oxygen uptake from the lungs into the blood. The virus does not infect a whole lung lobe, but scattered cells around the small blood vessels. These small blood vessels are involved in oxygen uptake. As a result, the virus induces limited lung damage with a maximum effect on oxygen uptake, much more than many other forms of pneunomia (Figure 6). This also influences the recovery after the lung disease: it takes longer for these cells to recover, causing prolonged recovery for ex-acute COVID-19 patients. Symptoms like low oxygen saturation and fatigue may persist for a long time.
Figure 6. Images of the lungs in healthy control and COVID-19.
Especially the small blood vessels (red) are affected, while the medium (yellow) and large blood vessels (blue) function normally.
Especially the small blood vessels (red) are affected, while the medium (yellow) and large blood vessels (blue) function normally.
Brain
More other coronaviruses, and even more than a third of the SARS-2 infected people will develop neurological symptoms. The mechanism of this is still unclear. Possibilities are:
- Virus infection of the brain
- Infection of nerve cells elsewhere in the body
- Thrombosis in the brain due to sepsis-like inflammation
- Precipitation of immune complexes
- Non-specific immune activation
- Autoimmune disease
- Fear
- Forgetfulness / dementia
- Mood swings / psychiatric complaints
- Fatigue
- Loss of smell and taste
- Balance problems
- Severe neurological complications, such as in a 37-year-old.
Inconspicuous complaints
About half of infected people fail to notice that they have corona, but some will develop complaints later. Covid complaints can differ strongly between individuals, but the reasons for this are not fully understood. Remarkably, the reports from outside China noticed more complaints than the early reports from China. One explanation is that the virus has mutated into variants that stay longer in the host, caused by the evolutionary pressure to infect more people.
Cardiac cells can be infected leading to chronic cardiac disease. Damage to the heart has been shown in various groups of people, including young athletes, but the bias of this research is sometimes disputed. Nevertheless, these studies provide important indications of what the (chronic) consequences of COVID-19 may be. Vascular infections and many small infarcts could damage various organs. The damage to lungs and / or ACE-2 cells - the oxygen detectors - can lead to long-term decreased oxygen in the blood circulation, reducing fitness of previous Covid patients.
All kinds of inflammatory reactions and immune complexes are seen in the kidneys that can lead to chronic complaints. In one study, mentioned that more than 1,000 patients required kidney transplantations.
In the pancreas, SARS-2 could infect the Langerhans’ islets leading to diabetes. These insulin-producing cells have ACE2 and are therefore sensitive to the SARS-2 virus when it enters the circulation. It is estimated that the incidence of novel diabetes increased with 80% due to the SARS-2 epidemic. With exception of diabetes, SARS-2 infection has no clear causal correlation with the development of autoimmune diseases. Some autoimmune diseases and rheumatism can be (temporarily) aggravated by the inflammatory symptoms.
SARS-2 could dysregulate the intestinal flora, reducing the number of commensals and increasing the number of pathogens. The permeability of the intestinal epithelium can also be increased, causing irritation and increasing vulnerability to infections. This could explain reported complaints of diarrhea (one in 6 or 5), nausea and vomiting (1 in 7). Loss of appetite is probably due to the combination of intestinal irritation and loss of smell and taste. About half of the patients shed virus in the stool after the respiratory disease has passed, sometimes up to 5 weeks later. In some patients, the concentrations are high, which would not exclude new infections through the fecal-oral route.
The inflammatory response can locally induce the ACE2 receptor, allowing the disease to enter a self-reinforcing circle.
Cardiac cells can be infected leading to chronic cardiac disease. Damage to the heart has been shown in various groups of people, including young athletes, but the bias of this research is sometimes disputed. Nevertheless, these studies provide important indications of what the (chronic) consequences of COVID-19 may be. Vascular infections and many small infarcts could damage various organs. The damage to lungs and / or ACE-2 cells - the oxygen detectors - can lead to long-term decreased oxygen in the blood circulation, reducing fitness of previous Covid patients.
All kinds of inflammatory reactions and immune complexes are seen in the kidneys that can lead to chronic complaints. In one study, mentioned that more than 1,000 patients required kidney transplantations.
In the pancreas, SARS-2 could infect the Langerhans’ islets leading to diabetes. These insulin-producing cells have ACE2 and are therefore sensitive to the SARS-2 virus when it enters the circulation. It is estimated that the incidence of novel diabetes increased with 80% due to the SARS-2 epidemic. With exception of diabetes, SARS-2 infection has no clear causal correlation with the development of autoimmune diseases. Some autoimmune diseases and rheumatism can be (temporarily) aggravated by the inflammatory symptoms.
SARS-2 could dysregulate the intestinal flora, reducing the number of commensals and increasing the number of pathogens. The permeability of the intestinal epithelium can also be increased, causing irritation and increasing vulnerability to infections. This could explain reported complaints of diarrhea (one in 6 or 5), nausea and vomiting (1 in 7). Loss of appetite is probably due to the combination of intestinal irritation and loss of smell and taste. About half of the patients shed virus in the stool after the respiratory disease has passed, sometimes up to 5 weeks later. In some patients, the concentrations are high, which would not exclude new infections through the fecal-oral route.
The inflammatory response can locally induce the ACE2 receptor, allowing the disease to enter a self-reinforcing circle.
Afterburner: Long covid
Early June 2020, Italian scientists reported that 5/6 hospitalized patients had still some health issues after two months after the start, and more than half of them had three or more complaints. Common symptoms were cough, fever, shortness of breath, joint pain, fatigue, intestinal complaints, loss of smell and taste. There are now 10.000s of cases of long haulers in the Netherlands, including a 22-year-old with eight months long-covid. The average disease-leave duration with COVID-19 is 8 weeks (55 days), but for 10% it is more than 200 days.
Long-covid, covid long haulers and post-acute sequelae of COVID-19 (PASC) are all names for a similar set of long-term symptoms. After three months, 1/3 has not recovered enough to return to normal work. This included British physicians. While age is a very large risk factor for death from COVID-19, this is less pronounced with long-term covid. Many young people may develop long covid.
A preliminary characterization of long covid shows how diverse these condition is:
Long-term symptoms of SARS-2 are mainly seen in cardiovascular disease, the lungs and the brain. Complaints after two and three months are dry cough, fatigue (especially extreme fatigue the day after exercise), shortness of breath, chest pain and low oxygen levels in the blood and sometimes new (bacterial) pneumonia develop. People also have headaches, concentration problems, forgetfulness, dizziness, anxiety, depression, and Post-Traumatic Stress Disorder (PTSD). Most other complaints are less common but can be very relevant. Many of these people are too severely affected to work. A number of these complaints are known from the post-ICU syndrome. This syndrome is known in people in the ICU with severe bacterial pneumonia - acute respiratory distress syndrome (ARDS). More than half of these ICU patients report new complaints after three and twelve months, including complaints such as breathlessness and dry cough (Figure 7).
Long-covid, covid long haulers and post-acute sequelae of COVID-19 (PASC) are all names for a similar set of long-term symptoms. After three months, 1/3 has not recovered enough to return to normal work. This included British physicians. While age is a very large risk factor for death from COVID-19, this is less pronounced with long-term covid. Many young people may develop long covid.
A preliminary characterization of long covid shows how diverse these condition is:
- Some have not recovered from the infection after 4, 8 and 12 weeks.
- Some have complications and organ damage after infection.
- Some are readmitted to hospital after having previously been discharged.
- Some are incapacitated for work due to lung covid and / or COVID-19 complications.
Long-term symptoms of SARS-2 are mainly seen in cardiovascular disease, the lungs and the brain. Complaints after two and three months are dry cough, fatigue (especially extreme fatigue the day after exercise), shortness of breath, chest pain and low oxygen levels in the blood and sometimes new (bacterial) pneumonia develop. People also have headaches, concentration problems, forgetfulness, dizziness, anxiety, depression, and Post-Traumatic Stress Disorder (PTSD). Most other complaints are less common but can be very relevant. Many of these people are too severely affected to work. A number of these complaints are known from the post-ICU syndrome. This syndrome is known in people in the ICU with severe bacterial pneumonia - acute respiratory distress syndrome (ARDS). More than half of these ICU patients report new complaints after three and twelve months, including complaints such as breathlessness and dry cough (Figure 7).
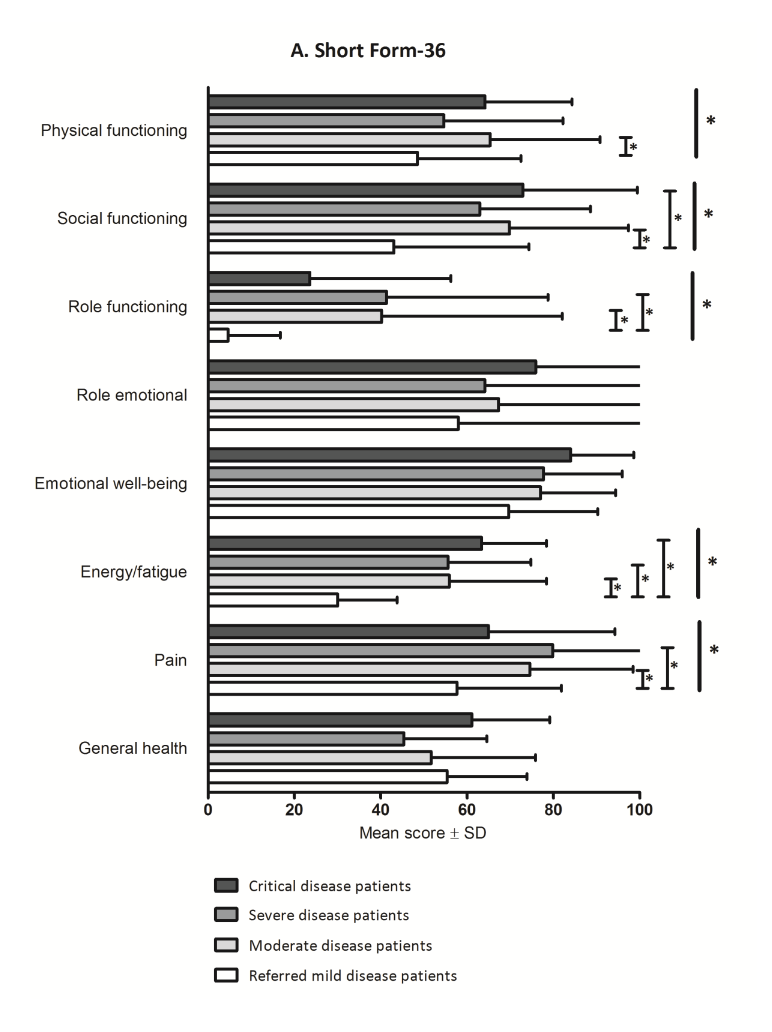
Figure 7. Complaints during and after acute COVID
Notable complaints
In contrast to the post-IC syndrome, many long-term COVID patients have not been admitted to the ICU (Figure 8). It is striking that the severity of the chronic complaints is not or hardly related to the severity of the acute illness. The reporting of the more serious complaints in the group with the mildest acute phase may be partially biased by the method of referring, but nevertheless indicates that serious acute disease is not a prerequisite to develop long covid. The complaints may last for 6 months or more, but the group decreases in size over time.
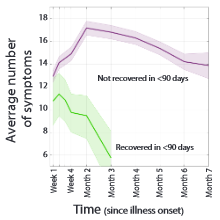
Focusing on subgroups, illustrates that people with (very) serious illness often do not have a long-term phase, while the moderate disease seems to be more often related to long-term effects (Figure 9A). Those that have not shown improvement after three months, may have still quite some symptoms after seven months. Although the number of complaints is slowly decreasing, averages of 17 and 14 symptoms at two and seven months after diagnosis, respectively, suggests that this might last for several years (Figure 9B).
Long-term complaints after SARS-2 infection differ strongly, maybe cause the virus can infect different tissues. The main hypotheses for long-covid are damage to the oxygen regulation system, an autoimmune disease, antibody complexes and persistent virus infection. Scientists want to create a working definition for long covid-related diseases. Such a definition or set of definitions is the basis for scientific research in to causes and mechanisms.
Focusing on subgroups, illustrates that people with (very) serious illness often do not have a long-term phase, while the moderate disease seems to be more often related to long-term effects (Figure 9A). Those that have not shown improvement after three months, may have still quite some symptoms after seven months. Although the number of complaints is slowly decreasing, averages of 17 and 14 symptoms at two and seven months after diagnosis, respectively, suggests that this might last for several years (Figure 9B).
Long-term complaints after SARS-2 infection differ strongly, maybe cause the virus can infect different tissues. The main hypotheses for long-covid are damage to the oxygen regulation system, an autoimmune disease, antibody complexes and persistent virus infection. Scientists want to create a working definition for long covid-related diseases. Such a definition or set of definitions is the basis for scientific research in to causes and mechanisms.
Figure 8. Various health parameters three months after 'recovery' from acute covid.
A score of 100% is normal functioning, 0% is not at all. From dark to slightly serious and less seriously ill patients from the hospital. The white group was not hospitalized but was later referred to the long covid policlinic
A score of 100% is normal functioning, 0% is not at all. From dark to slightly serious and less seriously ill patients from the hospital. The white group was not hospitalized but was later referred to the long covid policlinic
|
Figure 9A. Relationship between severity of acute and long-term COVID-19
|
Figure 9B. Number of symptoms people who did or did not recover from COVID within 3 months
|
What causes Long-Covid?
Pathology shows that the SARS-2 coronavirus causes much more symptoms than only pneumonia, it is a systemic infection. The virus causes significant chronic and acute damage in all organs, to a much wider extend than other diseases. It is unknown what causes of Long-Covid. Hypotheses include post-viral fatigue, autoimmune disease, and persistent virus infection. The symptoms are more severe than most post-viral fatigue. No antigen has been shown to be the target of autoimmune disease, but it has been shown that the virus persists in the body. People who were cured of COVID-19 three months before still have virus persistence in the intestines. SARS-2 may have a superantigen that causes persistent infection to cause fierce flare-ups of the disease.
Children
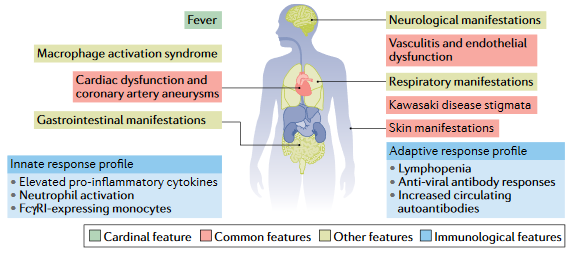
The multisystem inflammatory syndrome in adults (MIS-A) and children (MIS-C) is a life-threatening sepsis affecting many organs (Figure 10). Most adults also have pneumonia but many children were free of symptoms. Antibodies may be involved in several ways in MIS-C, the antibody receptors (FcγR) on monocytes and the activation of complement. The immune response causes damage to blood vessels. In MIS-C in children, the immune system is strongly activated, but for a short period. This may also activate inflammation at the blood vessels.
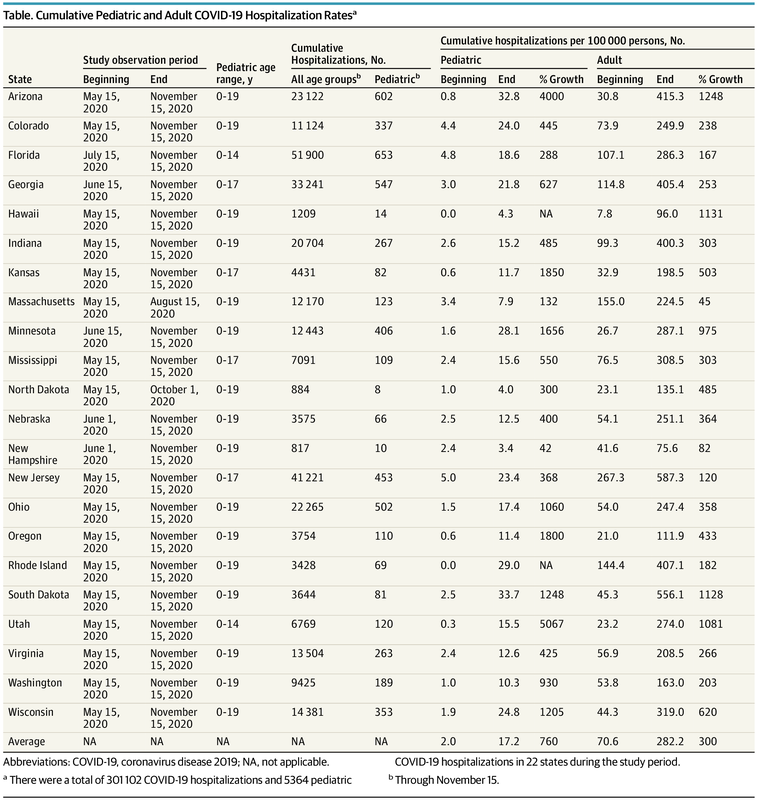
Recent US research shows that children may be regularly admitted to hospitals with COVID-19. Although less common than adults, corrected for their population, children are admitted 5% to 10% as often. Knowing that the mortality risks vary a factor 100 to 1000, this indicates that the disease is far from harmless in children (Figure 10). Notable are the large differences between states in the adult to child ratio, which could indicate different variants of virus circulating in different states (Figure 11). Of course, other explanations cannot be ruled out, so further research should confirm this.
Recent US research shows that children may be regularly admitted to hospitals with COVID-19. Although less common than adults, corrected for their population, children are admitted 5% to 10% as often. Knowing that the mortality risks vary a factor 100 to 1000, this indicates that the disease is far from harmless in children (Figure 10). Notable are the large differences between states in the adult to child ratio, which could indicate different variants of virus circulating in different states (Figure 11). Of course, other explanations cannot be ruled out, so further research should confirm this.
Figure 10. Clinical and immunological consequences of multisystem inflammatory syndrome in children (MIS-C)
Figure 11. Hospital admissions of children and adults
Age
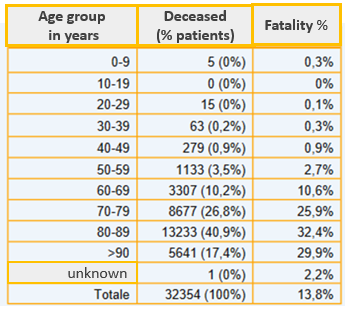
Just like almost all causes of death, SARS-2 affects older people more often than younger people, however, there has never been a reason to assume than children would be completely safe from this epidemic (Figure 16). From June 2020, it was clear that many people had long-term symptoms after they were released from the hospital and apparently cured.
Older people, sometimes referred to as people-of-a-day, have a high risk of dying, either from SARS-2 or from other diseases and comorbidities. All mortality is much lower in younger people. Although chances of death, co-morbidity, mortality from SARS-2 and long-term effects from SARS-2 in children are rare, they have a relatively large impact on children’s health. When acute and chronic mortality from SARS-2 is compared with other mortality by age group, SARS-2 appears to have an important contribution to disease and mortality for almost every age group. Because of the risks in children, AstraZeneca wants to look at vaccination of children between 6 and 17 years old.
Older people, sometimes referred to as people-of-a-day, have a high risk of dying, either from SARS-2 or from other diseases and comorbidities. All mortality is much lower in younger people. Although chances of death, co-morbidity, mortality from SARS-2 and long-term effects from SARS-2 in children are rare, they have a relatively large impact on children’s health. When acute and chronic mortality from SARS-2 is compared with other mortality by age group, SARS-2 appears to have an important contribution to disease and mortality for almost every age group. Because of the risks in children, AstraZeneca wants to look at vaccination of children between 6 and 17 years old.
Figure 12. Mortality by age group, early June 2020, Italy.
Fatal cases for children between 10 and 19 have now been reported in other studies.
Fatal cases for children between 10 and 19 have now been reported in other studies.
Air pollution deteriorates the disease.
Air pollution has an important contribution to the clinical cause of COVID-19, both in the acute and chronic phase:
The amount of particulate matter in the air varies from around 8 micrograms per cubic meter in the Northern Netherlands to about 12 micrograms in East Brabant and North Limburg. Wood stoves mainly emit ultrafine dust, which are smaller particles that reach deeper into the lungs and are more easily absorbed into the blood and brain than ordinary fine dust. Even though wood stoves mainly emit ultra-fine dust, they are responsible for 30 to 39% of the fine dust concentrations in residential areas. The concentration of particulate matter produced by stoves is then 2.5 to 5 μg / m3. In comparison, 1 μg / m3 increases the risk of COVID-19 by a factor of 9.4, of hospital admissions by a factor of 3 and mortality by a factor of 2.3. Simple multiplication then yields almost a factor of 6 to 12 higher mortality due to wood smoke alone, apart from other air pollution. Reducing air pollution, especially in residential areas, therefore has a major impact on COVID-19 mortality. The ban on wood burning could therefore be an effective measure against death from COVID-19.
- Air pollution causes chronic diseases such as asthma, COPD, lung cancer, heart disease and diabetes. Many of these conditions are prone to COVID-19 hospitalization, ICU admission and death.
- Air pollution reduces the resistance of the respiratory tract to bacterial and viral infections. People living in areas with a lot of pollution may be infected more often and develop more severe disease.
- Many COVID-19 survivors yield comorbidity at the heart, lungs, and other organ systems due to air pollution. Social inequality also plays a role here for people who live in more polluted areas.
- The impact of air pollution on heart and chronic lung disease is more than significant enough to make a strong case for cleaner air for health reasons.
The amount of particulate matter in the air varies from around 8 micrograms per cubic meter in the Northern Netherlands to about 12 micrograms in East Brabant and North Limburg. Wood stoves mainly emit ultrafine dust, which are smaller particles that reach deeper into the lungs and are more easily absorbed into the blood and brain than ordinary fine dust. Even though wood stoves mainly emit ultra-fine dust, they are responsible for 30 to 39% of the fine dust concentrations in residential areas. The concentration of particulate matter produced by stoves is then 2.5 to 5 μg / m3. In comparison, 1 μg / m3 increases the risk of COVID-19 by a factor of 9.4, of hospital admissions by a factor of 3 and mortality by a factor of 2.3. Simple multiplication then yields almost a factor of 6 to 12 higher mortality due to wood smoke alone, apart from other air pollution. Reducing air pollution, especially in residential areas, therefore has a major impact on COVID-19 mortality. The ban on wood burning could therefore be an effective measure against death from COVID-19.